Alcoholic liver disease has more bleeding tendency during liver transplant operation in low MELD patients ≤ 20
Mun Chae Choi1, Jae Geun Lee1,2, Juhan Lee1,2, Seok Jeong Yang1, Myoung Soo Kim1,2, Soon Il Kim1,2, Dong Jin Joo1,2.
1Department of Surgery, Yonsei University College of Medicine, Seoul, Korea; 2The Research Institute for Transplantation, Yonsei University College of Medicine, Seoul, Korea
Introduction: Alcohol Liver Disease (ALD) includes a wide clinical spectrum from acute alcoholic hepatitis to severe cirrhosis and/or hepatocellular carcinoma. Many liver surgeons agree that liver transplantation for those with ALD is harder than other etiologies such as viral hepatitis. Until now, there was no report to reveal the bleeding tendency of ALD compared to other diseases in a transplant operation. Thus, we analyzed the blood loss and transfusion amount during operation according to the etiologies of liver disease.
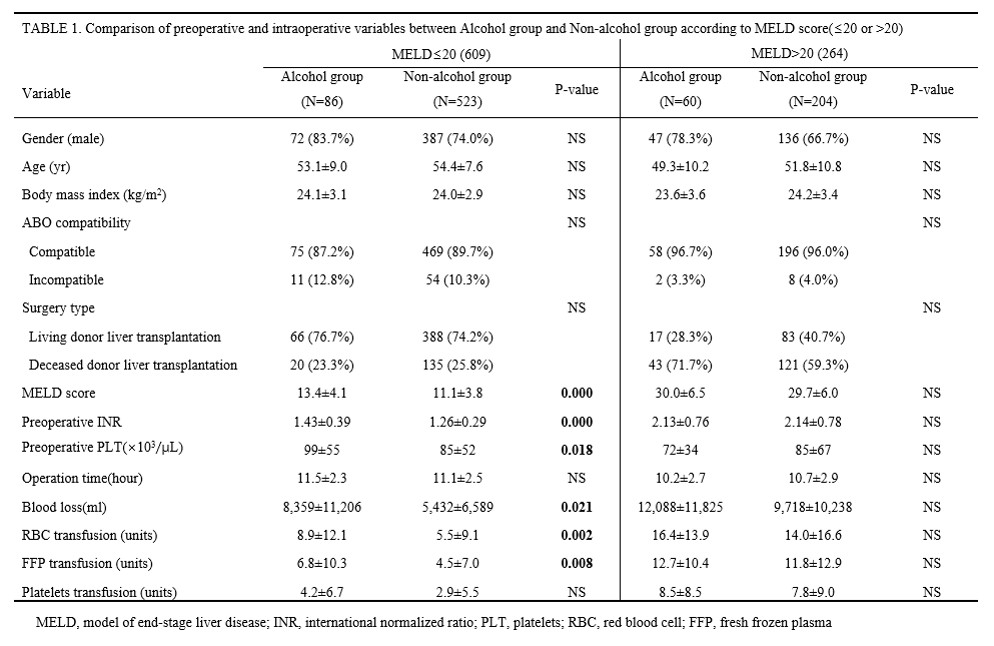
Patients and Methods: The data from 873 patients who underwent liver transplant (LT) in our center were retrospectively collected and analyzed. We compared recipients’ gender, age, BMI, ABO compatibility, LDLT vs DDLT, preoperative INR, platelet counts, operation time, blood loss during operation, and transfusion amounts between ALD and Non-ALD.
Results: Out of 873 LT patients, 264 patients had higher MELD score than 20 at the time of LT, while 609 patients under MELD 20. Among the lower MELD group, the number of ALD was 86 (14.1%) and the higher MELD group had 60 ALD (22.7%).
In the lower MELD group, the ALD group showed higher preoperative INR than the Non-ALD group (1.43±0.39 Vs. 1.26±0.29, P<0.001). But preoperative platelet count of the ALD group was higher than the Non-ALD group (99±55 Vs. 85±52, P=0.018). Operation time was not different. Blood loss, RBC, and FFP transfusion of ALD group were significantly higher than Non-ALD group even in the lower MELD group (8,359±11,206 mL Vs. 5,432±6,589 mL, P=0.021; 8.9±12.1 unit Vs. 5.5±9.1, P=0.002; 6.8±10.3 unit Vs. 4.5±7.0 unit, P=0.008, respectively). However, higher MELD group (>20) showed no significant difference between ALD and Non-ALD group.
Conclusion: ALD showed more bleeding tendency than Non-ALD during LT operation. These findings imply that transplant surgeon need to prepare for blood loss during operation for ALD patients, who have even lower MELD scores.
There are no comments yet...