Survival benefits of living donor liver transplant for hepatorenal syndrome candidates on waitlist
Tiffany Cho-Lam Wong1, James Fung2, Jeff Dai1, SL Sin1, Brian She1, Albert Chan1, TT Cheung1, CM Lo1.
1Surgery, The University of Hong Kong, Hong Kong, Hong Kong; 2Medicine, The University of Hong Kong, Hong Kong, Hong Kong
Introduction: The utilization of living donor liver transplant (LDLT) for candidates with hepatorenal syndrome (HRS) is controversial.
Method: This was a retrospective study from the University of Hong Kong. All data was retrieved from a prospective collected database. All liver transplant candidates who were accepted on waitlist from 2008 to 2017 were analyzed. Patients were divided into 2 groups. For candidates who had at least one potential live donor, they would be considered as “intention-to-treat LDLT group” (ITT-LDLT). Whereas patients who had no live donor would belong to “intention-to-treat DDLT group” (ITT-DDLT).
HRS was defined as acute kidney injury (AKI) in patients with cirrhosis after ruling out other causes of AKI. All patients were treated with intravenous albumin and terlipressin, +/- renal replacement therapy.
Primary outcome was to compare the ITT-overall survival for ITT-LDLT vs. ITT-DDLT for candidates with HRS.
Results: 992 patients were listed (496 in ITT-LDLT and 496 in ITT-DDLT). 352(36.6%) patients had HRS. Baseline characteristics of all patients were listed in table 1. Patients in ITT-LDLT HRS. There were more femlae in ITT-LDLT group and they were sicker (higher MELD and more ICU candidates). The overall survival of ITT-LDLT was better than ITT-DDLT in HRS canddiates. (Figure 1). The 1-,3- and 5-year survival was 66.5% 59.5% and 58.7% in ITT-LDLT HRS and they were 54.6%, 41.4% and 39.4% in ITT-DDLT HRS (p<0.001).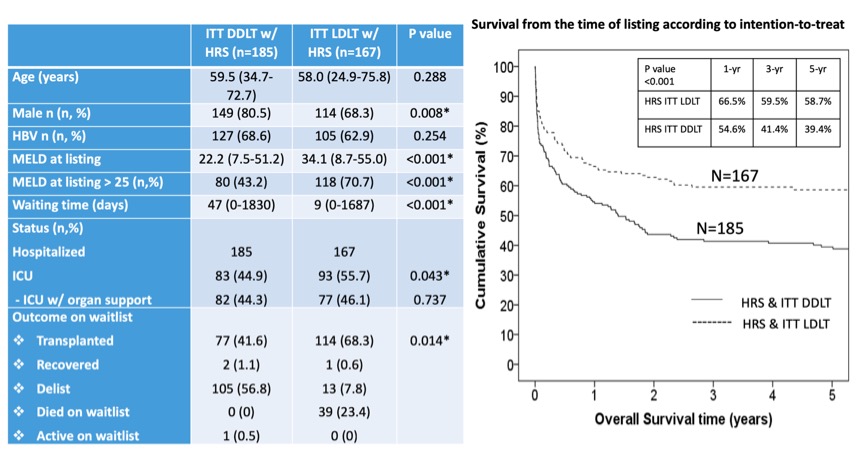
191 patients (DDLT n=116, LDLT n=75) underwent liver transplant. There was no difference in perioperative outcomes including mortality and morbidity between the 2 groups. Post transplant survival at 1-.3- and 5-year were also similar.
Conclusion: The was the 1st study to show that with ITT analysis, ITT-LDLT offered significant survival benefits than ITT-DDLT in HRS patients. Waitlist dropout/ mortality should be consdiered and ITT-LDLT allowed a timely access to transplant. Similar perioperative and post-transplant outcomes suggested LDLT was justified in HRS patients.