Normothermic machine perfusion of marginal liver allografts is associated with a low incidence of post reperfusion syndrome in high risk recipients
Angus Hann1, Hanns Lembach1, Amanda Carvalheiro1, Youri Boteon1, Siobhan McKay1, Prashant Kadam1, Buddika Dissanayake1, Suchintha Tilakaratne1, Mohammad Alzoubi1, David Bartlett1, Asif Arshad2, Hentie Cilliers2, Suresh Vasanth2, Gowri Subash2, Thomas Faulkner2, Rachel Moore2, James Cuell2, Rajashankar Rao2, Davinia Bennet2, John Isaac2, Nick Murphy2, Scott Russel2, Naveed Javed2, Asim Iqbal2, Keith Roberts1, Andrea Schlegel1, Thamara Perera1.
1Liver transplant and hepatobiliary surgery unit, UHB NHS Foundation trust, Birmingham, United Kingdom; 2Department of anaesthesia, UHB NHS Foundation trust, Birmingham, United Kingdom
Introduction: Post reperfusion syndrome (PRS) in liver transplantation (LT) is associated with worse outcomes. We describe the post reperfusion characteristics of marginal grafts that subsequently underwent normothermic machine perfusion (NMP) and implantation into high-risk recipients.
Materials and Methods: Adult patients that received an NMP preserved DBD graft as part of The NAPLES (Normothermic mAchine Perfusion of Liver to Enable high riSk recipients) project were included. The Organox Metra device was utilised and grafts perfused for a minimum of four hours and those fulfilled previously established viability criteria were transplanted. Donor, graft, recipient and relevant intraoperative variables were prospectively collected. PRS was defined as a sustained fall in mean arterial pressure (MAP) by more than 30% within the first 5 minutes after reperfusion.
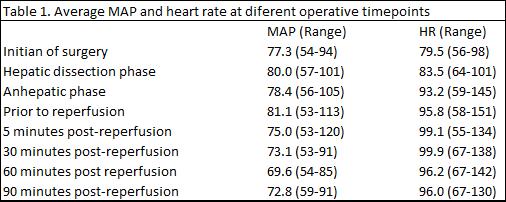
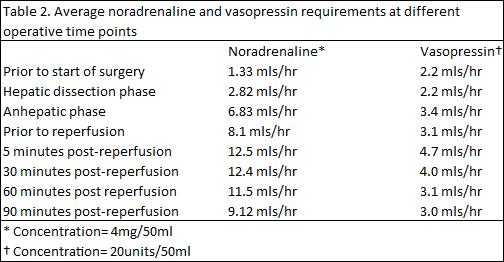
Results: Twenty-six patients received NMP preserved DBD grafts between December 2018 and March 2020. Median donor age (51; 29-78) and 17/26 (65.4%) were steatotic. 15/26 were regraft candidates whilst others were technically challenging patients including complex PVT. The median cold ischaemic time, NMP and total preservation time were 370 (127-638), 720 (251-1383) and 1073 (578-1837) minutes respectively. A reduction in MAP occurred on reperfusion in 14 (54%) of subjects however only 3/26 (11%) patients developed clinically significant PRS (11.5%). The haemodynamic changes and vasopressor requirements are displayed in table 1 and table 2 respectively. Mean arterial pressure changes were ≤15%, 15-30% and ≥30% in 5, 6 and 3 subjects respectively.
Discussion: Despite pushing the boundaries in LT with marginal grafts in highest risk candidates, the incidence of PRS is in keeping with the reported incidence that range between 12% - 49% following static cold storage.1 The majority of the grafts were considered high risk and declined by other centres, as these were thought to be higher risk for PRS. PRS is generally considered to occur due to a massive efflux of the inflammatory cytokines, reactive oxygen species and vasoactive agents from the graft.2 These are all potentially generated during the ischaemic organ preservation period. Significant haemodynamic changes still occurred with these NMP preserved grafts. However, we feel that NMP mitigates this ischaemic insult and is associated with a better reperfusion profile.
Conclusion: The reperfusion phase of a liver transplant is a critical point that is frequently associated with haemodynamic instability and possible cardiac arrest. In this study, NMP preservation of marginal liver grafts resulted in a low incidence of PRS in this cohort of high-risk recipients.
[1] 1. Siniscalchi A, Gamberini L, Laici C, Bardi T, Ercolani G, Lorenzini L, et al. Post reperfusion syndrome during liver transplantation: From pathophysiology to therapy and preventive strategies. World journal of gastroenterology. 2016;22(4):1551-69.
[2] 2. Manning MW, Kumar PA, Maheshwari K, Arora H. Post-Reperfusion Syndrome in Liver Transplantation-An Overview. J Cardiothorac Vasc Anesth. 2020;34(2):501-11