Settling the difference: Analysis of kidney graft function discordance at transplant from deceased donor paired kidneys
Essa Abuhelaiqa1, Mohamad M. Alkadi1, Shafik Mansour2, Litty Mathew3, Faten Makableh3, Awais Nauman1, Omar Fituri1, Muhammad Asim1, Omar I. Ali3, Riadh Fadhil3, Yousif Al Maslamani3, Hassan Al-Malki1.
1Nephrology, HMC, Doha, Qatar; 2Medicine, HMC, Doha, Qatar; 3Transplant Surgery, HMC, Doha, Qatar
Introduction: Analysis of paired kidneys from deceased donors has the advantage of eliminating donor and center related biases seen in previous studies that evaluated kidney graft function and graft outcomes. Our center has the advantage of having a single organ procurement organization and the only transplant center for the whole country. This study aims to evaluate recipient risk factors that lead to discordant low eGFR of deceased kidney pairs at the early post-transplant period and evaluate long term outcomes of the discordant kidneys.
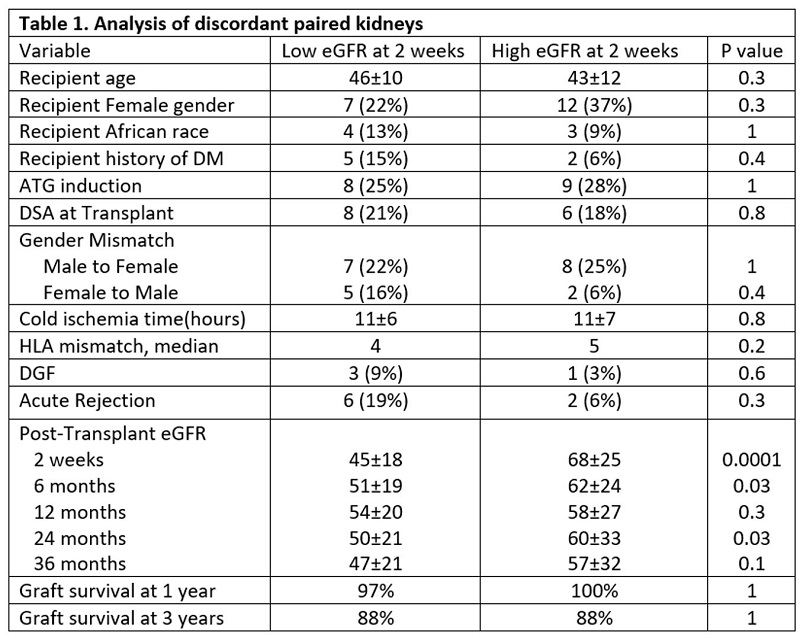
Materials and Methods: We retrospectively evaluated deceased donors transplants between 2010-2017. There were 64 kidney pairs from 32 deceased donors (mean age: 41 years, 16% female, and 13% had KDPI >85%). Kidney function was calculated at 2 weeks post transplant using CKD-EPI formula. Discordant pairs with eGFR difference more than 5 mL/min were divided into low eGFR group and high eGFR groups. Donor and recipient variables were analyzed between the two groups using Wilcoxon and chi square tests for continuous and categorical variables, respectively.
Results and Discussion: All pairs had discordance in eGFR more than 5 mL/min and majority (75%) had eGFR discordance more than 10 mL/min post transplant which suggest that despite having similar donor variables, kidney function at transplant is signficantly different. We did not observe a difference in age, gender or race as shown in table 1, hence recipient variables may not have a significant role to the obesrved difference in our cohort. Preformed DSA were present and delayed graft function occurred more frequently in low eGFR but were not significant (21% vs. 18%, P=0.9 and 9% vs. 3%, P=0.3, respectively), suggesting that the oberseved eGFR difference may be related to ischemia reperfusion or antibody injury. Acute rejection was also more frequent in low eGFR (19% vs. 6%, P=0.3). The mean eGFR difference between the two groups decreased after 6 months and graft survival was not different as shown in figure 1 and figure 2, respectively. The impact of discordant kidney function was not signifcant in the long term follow up in our cohort, infact many paired kidneys became concordant.
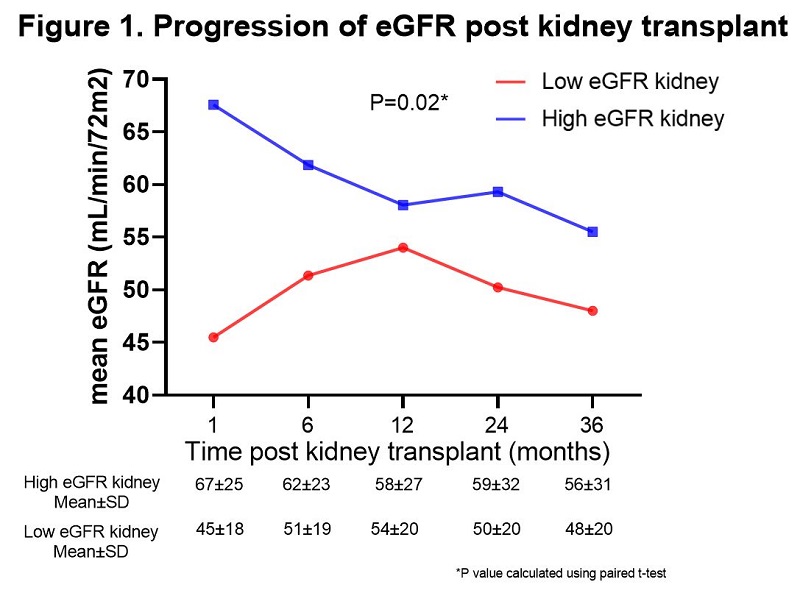
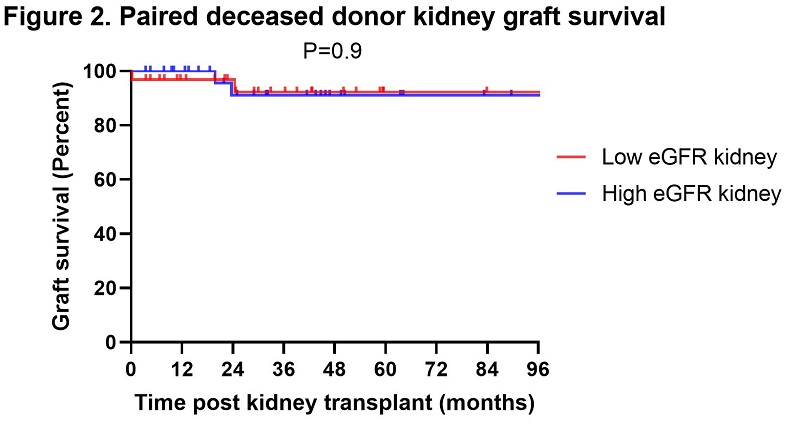
Conclusions: Our single center analysis of paired deceased donor transplants demonstrated that a decrease in initial renal function may be associated with immunologic and ischemia reperfusion injury. However, despite a difference in kidney function at the time of transplant and recipient variables, both paired kidney functions normalize and perform well over long term follow up.