Marginal livers have excellent outcomes in pediatric patients with metabolic liver disease
Christine Hwang1, Cyrus Feizpour1, Amal Aqul2, Dev Desai1, Steven Hanish1, Lucia De Gregorio1, Parsia Vagefi1, Malcolm MacConmara1.
1Surgery, UT Southwestern Medical Center, Dallas, TX, United States; 2Pediatrics, UT Southwestern Medical Center, Dallas, TX, United States
Introduction: Pediatric patients with metabolic diseases are listed so that livers are preferentially allocated to them, having the option of receiving very high quality organs. We examined outcomes of these livers in comparison to livers with marginal characteristics to see if a pediatric metabolic recipient should wait for a prime organ.
Methods: The UNOS database was queried to examine outcomes in all pediatric liver transplant recipients (<18 years) who were transplanted between 1987 - 2018. Living donor and multi-organ recipients were excluded. Patients with a diagnosis of glycogen storage disease (GSD) type I, GSD type IV, homozygous hypercholesterolemia, tyrosinemia, hyperoxaluria, maple syrup urine disease, and “other” metabolic diseases were included for analysis. A marginal liver was defined as one with any of the following characteristics: donor age > 60 years, terminal transaminases > 500 U/L, biopsy proven macrosteatosis > 30%, cold ischemia time (CIT) > 8 hours, donation after cardiac death (DCD) donor, or HBV core Ab +/HCV Ab + donor. Donor and recipient demographic data were examined, as were survival and outcomes. A p-value of <0.05 was considered to be significant.
Results: There were 1342 metabolic pediatric patients who underwent liver transplantation; 926 received a high quality (HQ) liver; 416 received a marginal (MARG) liver. The MARG donor was significantly younger (9.9 vs. 12.9 years), had a lower BMI (18.9 vs. 20.0 kg/m2), a higher SGPT (64.2 vs. 53.1) and SGOT (107.6 vs. 70.9), longer CIT (11.0 vs. 5.5 hours), and higher DCD percentage (1.0% vs. 0%). Recipients of MARG livers were not significantly different in age (4.8 vs. 4.5 years), BMI (18.7 kg/m2vs. 18.7 kg/m2), final MELD/PELD score (2.8 vs. 1.8), or wait time (150.2 vs. 168.6 days). MARG liver recipients were more likely to be on life support (8.9% vs. 6.0%, p<0.05), and trended to having a longer length of stay (45.1 vs. 24.4 days, p=0.05). Outcomes showed similar or improved outcomes when examining causes of allograft failure including primary nonfunction, acute or chronic rejection, and thrombotic events. When allograft survival was examined, there was no difference when comparing HQ vs. MARG livers (Figure 1).
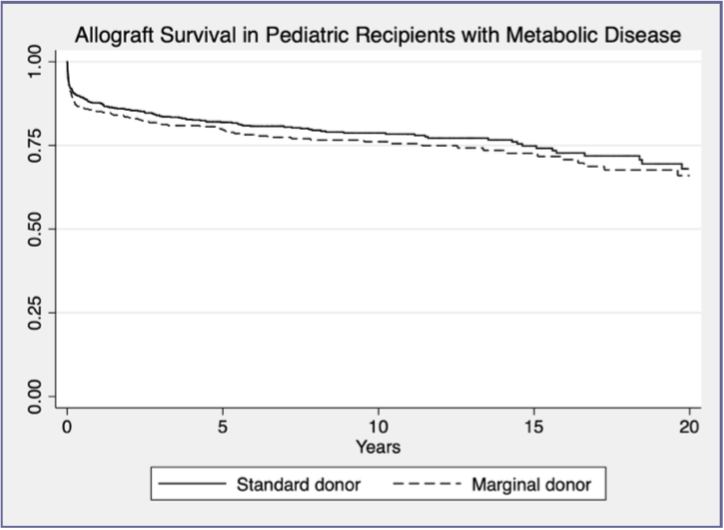
Conclusions: Livers with marginal characteristics have similar allograft outcomes and survival when compared to high quality livers that are transplanted into pediatric metabolic recipients. Rather than waiting for the perfect liver, it should be strongly considered to transplant a liver with expanded criteria characteristics into these patients as long term allograft survival does not suffer.