Significance of sarcopenia in infants with pediatric liver transplantation for biliary atresia
Masahiro Takeda1, Seisuke Sakamoto1, Hajime Uchida1, Seiichi Shimizu1, Yusuke Yanagi1, Akinari Fukuda1, Shunsuke Nosaka2, Mureo Kasahara1.
1Organ Transplantation Center, National Center for Child Health and Development, Tokyo, Japan; 2Department of Radiology, National Center for Child Health and Development, Tokyo, Japan
Background: While sarcopenia, the disproportionate loss of muscle mass, is a significant predictor of liver transplantation (LT) outcomes in adults, few studies have examined the association of sarcopenia in pediatric patients with LT for biliary atresia (BA). We hypothesized that the assessment of core muscle mass may serve as a new prognostic marker of LT outcomes and index of malnutrition in infants with BA. The present study aimed to investigate the clinical significance of sarcopenia for LT outcomes in infants with BA.
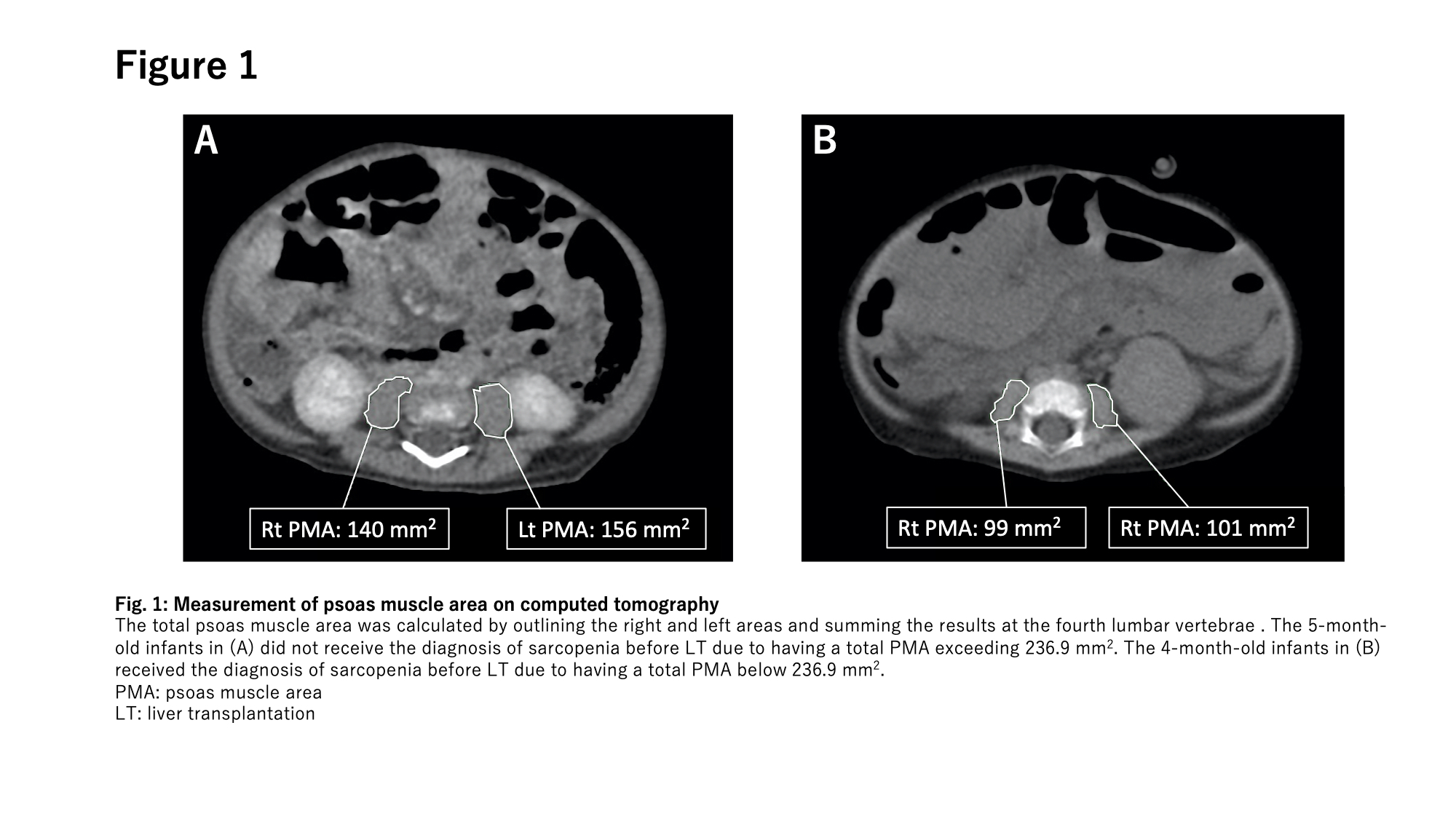
Patients and Methods: To define sarcopenia in infants, the cross-sectional area of the total psoas muscle (PMA) in 93 healthy control infants was measured by computer tomography (Figure 1). Sarcopenia was defined as a total PMA lower than two standard deviations below the mean of the healthy control group. Eighty-nine infants with BA with the median age at LT of 7.6 months between 2005 and 2018 were enrolled. The patients were divided into the sarcopenia group (n=21) and non-sarcopenia group (n=68), and their preoperative characteristics, postoperative complications, incidence of infection, length of hospital stay, ICU stay, postoperative ventilator duration and the patient / graft survival rate were analyzed.
Results: The patients’ weight and height and the proportion of z-scores < -1.5 for weight and height did not significantly differ between the two groups (Table 1).
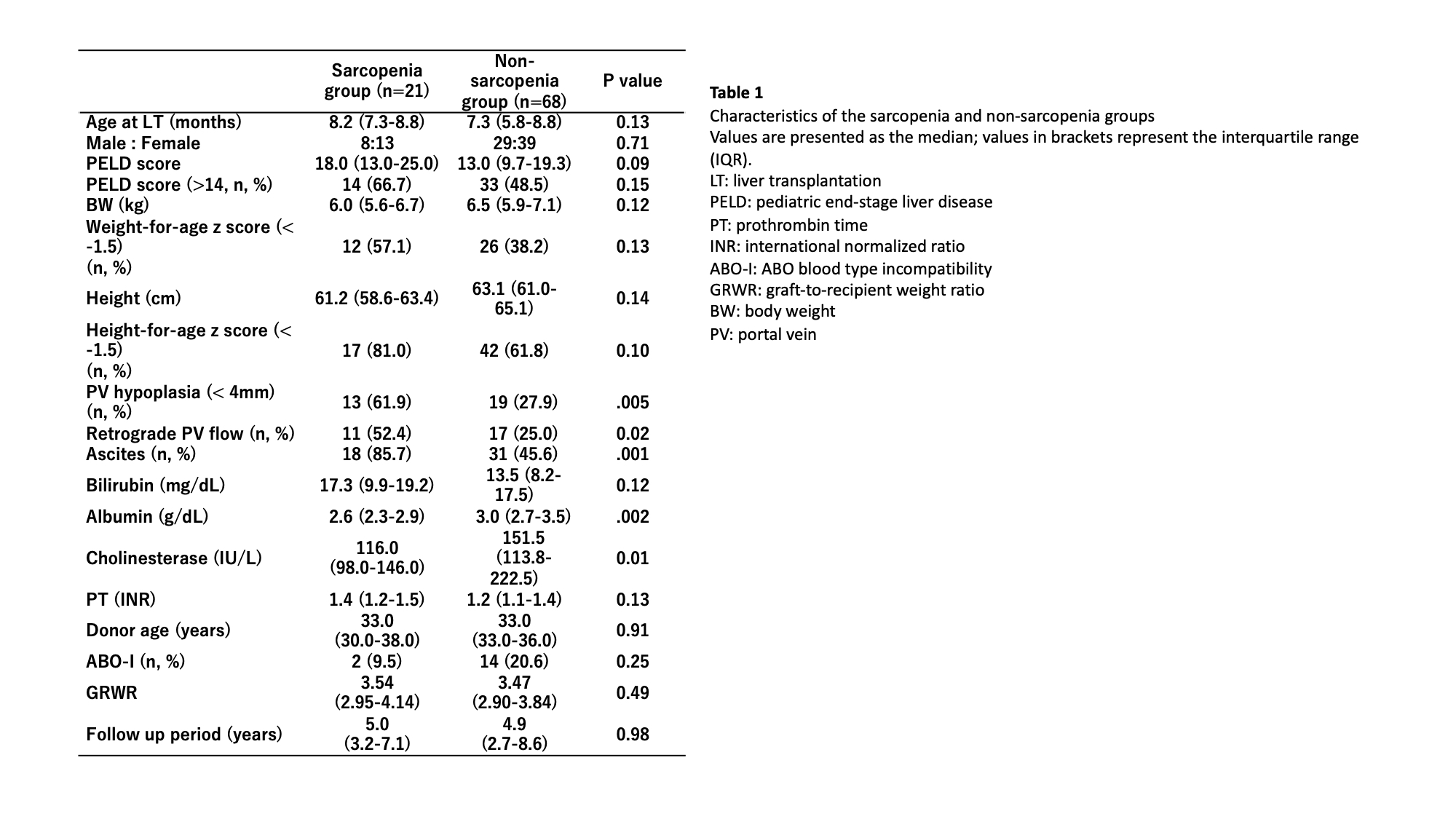
The rate of portal vein (PV) hypoplasia, retrograde PV flow, and preoperative ascites were significantly higher in the sarcopenia group (p=.005, 0.02 and .001 in each). The sarcopenia group had a significantly longer operation time and greater blood loss during LT (511.0 minutes vs. 476.0 minutes, p=0.03 and 108.8 g/kg vs. 76.4 g/kg, p=0.02) (Table 2).
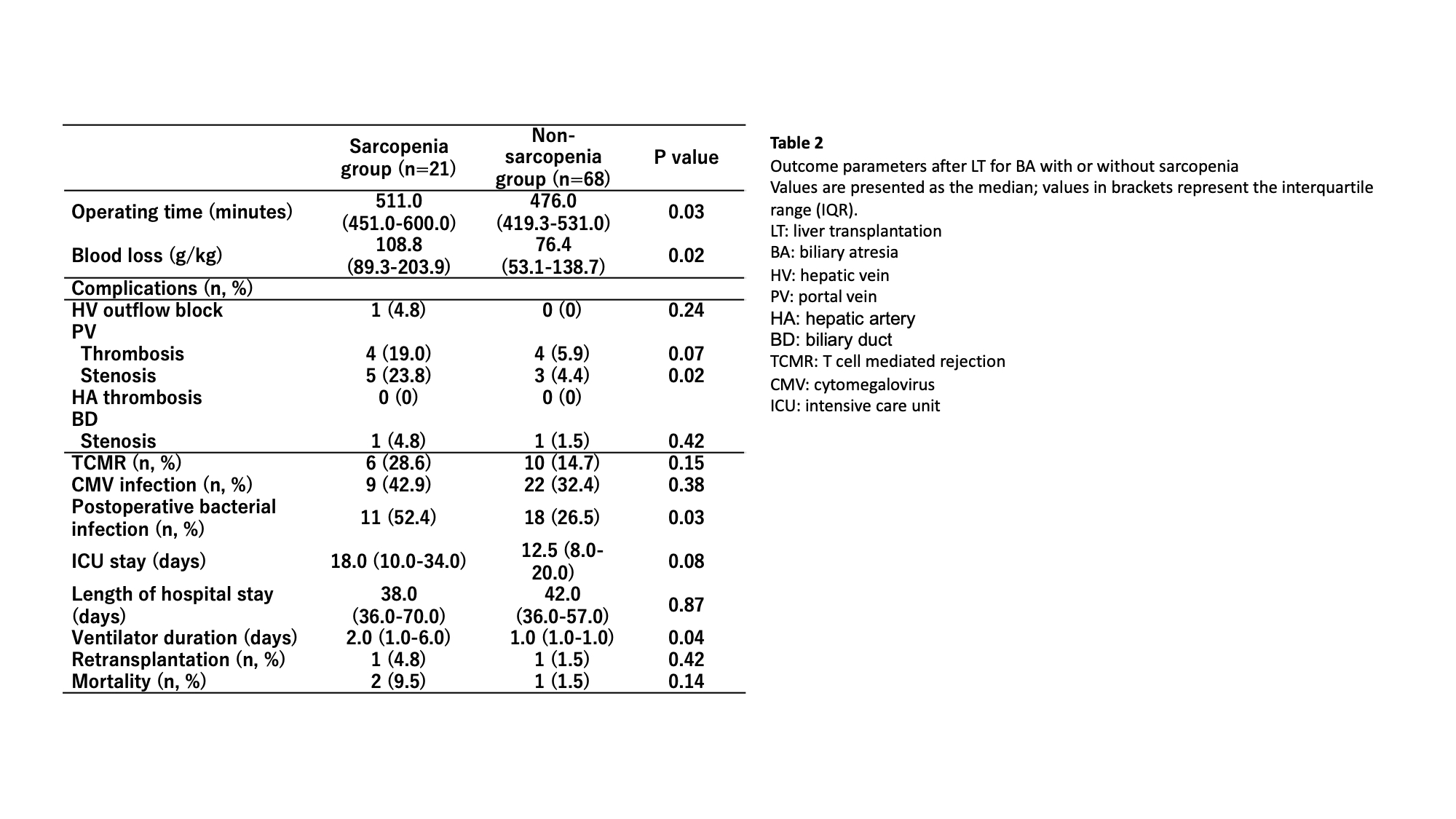
The incidence of PV stenosis and postoperative bacterial infection was also significantly higher in the sarcopenia group (23.8% vs. 4.4%, p=0.02 and 52.4% vs. 26.5%, p=0.03, respectively). The total length of hospital stay between the two groups did not differ significantly (p=0.87). The one-year patient and graft survival rates in the sarcopenia group tended to be lower (sarcopenia group: 90.5% vs. non-sarcopenia group: 98.5%, p=0.07 and 85.7% vs. 97.1%, p=0.05, respectively) (Figure 2).
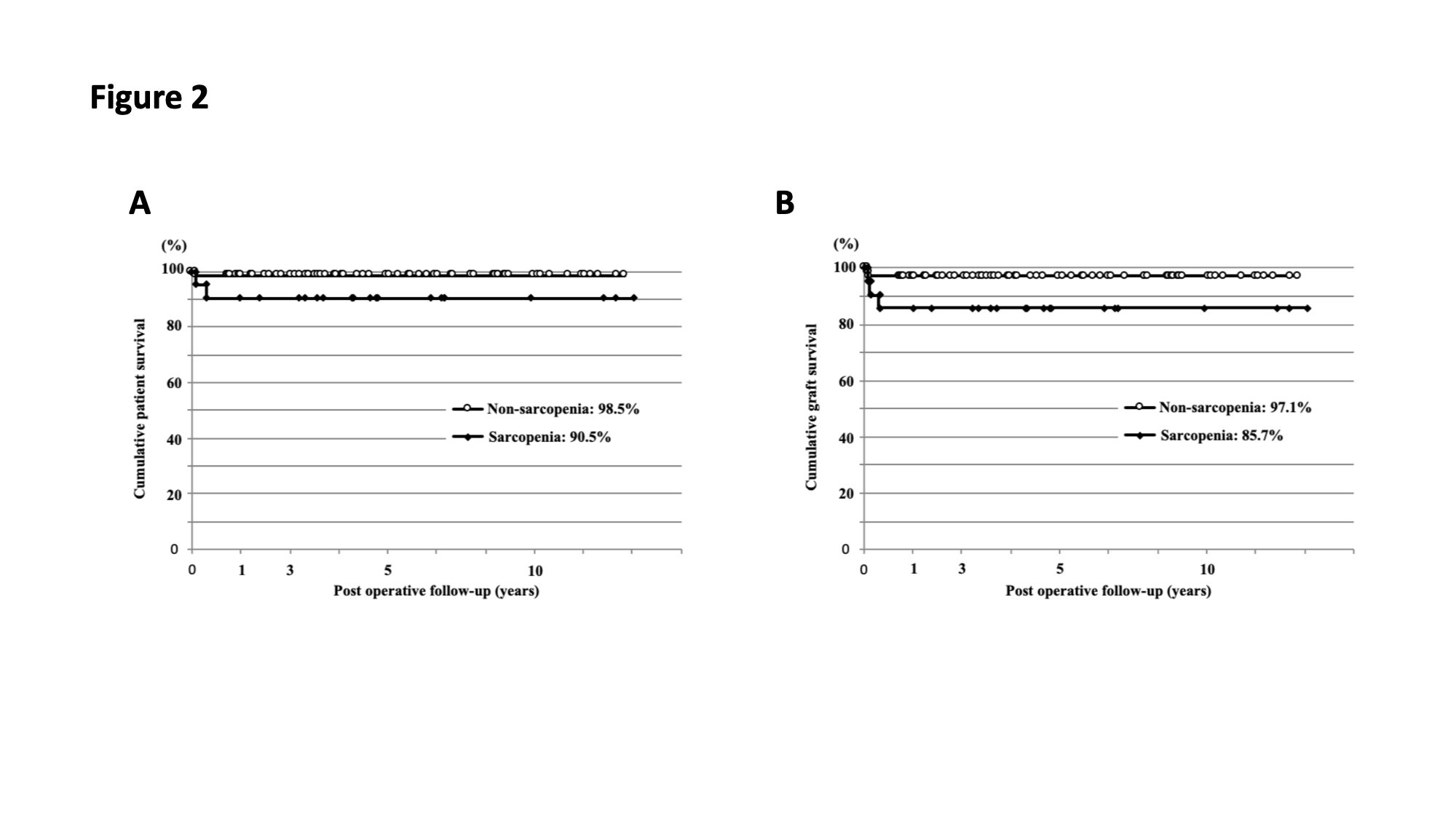
Conclusions: Sarcopenia in infants with BA before LT may be associated with patient survival and serve as a new and effective prognostic marker for growth retardation and postoperative outcomes of LT.