A recent diagnosis of tuberculosis is a risk factor for post-transplant morbidity & mortality after liver transplantation: A propensity score match-based analysis
Pradez Sapkota1, Ashwin Rammohan1, Mukul Vij2, Naresh Shanmugan3, Dinesh Jothimani4, Mettu S. Reddy1, Mohamed Rela1.
1HPB and Liver Transplantation, Dr. Rela Institute and Medical Center, Chennai, India; 2Department of Pathology, Dr. Rela Institute and Medical Center, Chennai, India; 3Department of Pediatric Hepatology, Dr. Rela Institute and Medical Center, Chennai, India; 4Hepatology, Dr. Rela Institure and Medical Center, Chennai, India
Background: Tuberculosis (TB) remains a major health care issue in South Asia. It’s impact on outcomes after liver transplantation (LT) needs greater attention as LT becomes increasingly available here.
Methods: All patient undergoing LT in our centre between Jan 2010 and September 2019 with a history of TB were identified and divided into two groups - TB diagnosed and treated > 6 months ago (TBold) and TB diagnosed within 6 months or during LT(TBactive). TBold & TBactive cohorts were matched to recipients without TB (Control) in a 1:2 ratio using propensity score matching (PSM). Recipient age, gender, MELD, donor age, transplant-year and procedure-type (DDLT/LDLT) were the matching parameters. Post-op outcomes and mortality were compared between TBold, TBactive and Control groups.
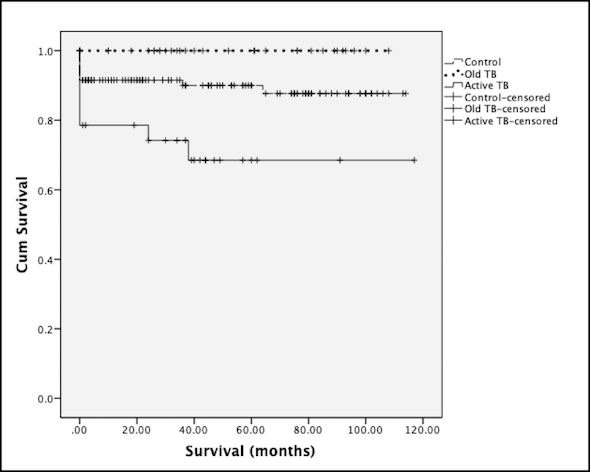
Results: 50 of 1280 LT recipients (3.9%) had a history of TB (TBold: 30, TBactive:20). There was no difference in recipient age& gender, donor age, procedure-type & GRWR (for LDLT) between TBactive & TBold cohorts. MELD for TBactive was higher (20.7±6.2 vs 16.2±6.6, p=0.025) compared to TBold. When compared to TBold cohort, TBactive had more post-transplant morbidity (Clavien>grade 2, 75% vs 43.3%, OR:3.93, 95%ci 1.13,13.6; p=0.042) & poorer 90-day survival (70% vs 100%, p=0.002). When compared with PSM-matched controls, TBactive had higher morbidity (75% vs 34.7%,OR:5.6(95%ci 1.9,16.6, p=0.001) and poorer 90-day survival (70% vs 91.5%,p=0.014). There was no difference in outcomes between TBold & PSM matched controls. Active TB was identified as a risk factor for mortality (OR:0.19;p=0.002). Overall survival of TBactive cohort was poorer than TBold & control groups (log rank test, p=0.002) (Figure).
Conclusion: Active TB in the peri-transplant period is a risk factor for post-transplant morbidity, early mortality & overall survival.
[1] Holty JE. Liver Transpl. 2009 Aug;15(8)
[2] A. Olithselven AASLD 2014
[3] A. Subramanian 2019 uptodate