Intraoperative low-dose dexmedetomidine attenuates hepatic ischemia-reperfusion injury in pediatric living donor liver transplantation
Liang Zhang1, Wenhe Yang1, Fushan Xue1, Azmat Riaz2, Zhijun Zhu3,4,5.
1Anesthesiology, Beijing Friendship Hospital, Capital Medical University, Beijing, People's Republic of China; 2Anesthesiology, Pak-Emirates Military Hospital, Rawalpindi, Pakistan; 3Liver Transplantation, Beijing Friendship Hospital, Capital Medical University, Beijing, People's Republic of China; 4Clinical Center for Pediatric Liver Transplantation, Capital Medical University, Beijing, People's Republic of China; 5Liver Transplantation Center, National Clinical Research Center for Digestive Diseases, Beijing, People's Republic of China
Background: Dexmedetomidine (DEX) is an anesthetic adjuvant increasingly used in pediatric anesthesia. However, the impact of low-dose DEX on postoperative liver graft function in pediatric living donor liver transplantation (LDLT) is still unclear. The objective of this retrospective study was to explore its potential hepatoprotective effect in pediatric LDLT.
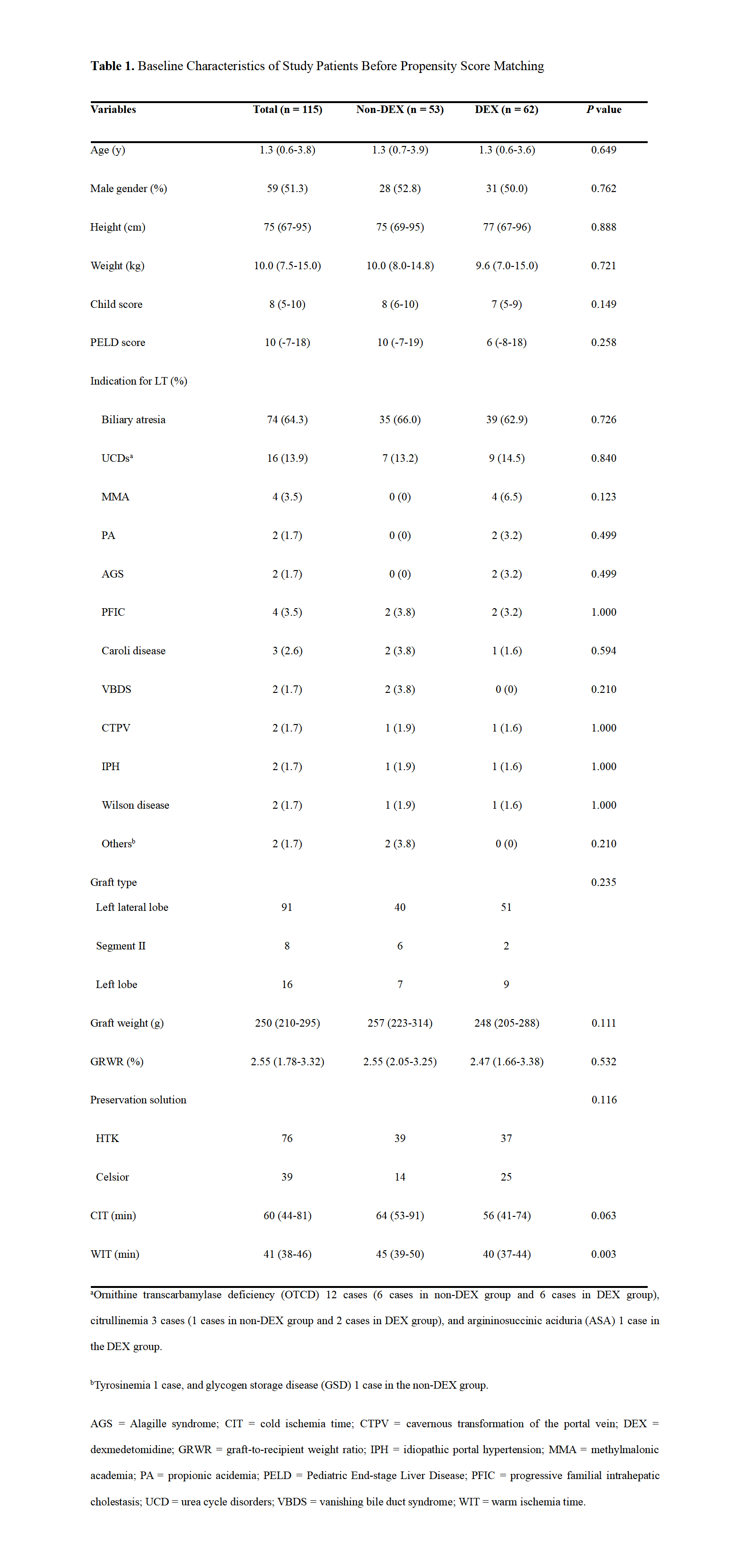
Methods: A retrospective study of 115 pediatric patients submitted to LDLT from January 2016 to December 2018 was conducted. Patients were stratified into DEX and non-DEX groups according to intraoperative DEX use and different time periods in our hospital. Patients in the DEX group (n = 62) received an additional infusion of DEX at the rate of 0.4 μg/kg/h compared with those in the Non-DEX group (n = 53). Data on postoperative liver graft function and other variables were collected and compared. Propensity score (PS) matching analysis was designed to control selection bias. Independent predictors of moderate-to-extreme hepatic ischemia-reperfusion injury (HIRI) were identified by binary logistic regression.
Results: The DEX group showed lower postoperative peak alanine aminotransferase, aspartate aminotransferase, lactic dehydrogenase, and blood urea nitrogen levels (All P<0.05), less frequent development of moderate-to-extreme HIRI (P = .013), and shorter duration of hospital stay (P = .011) than the non-DEX group.
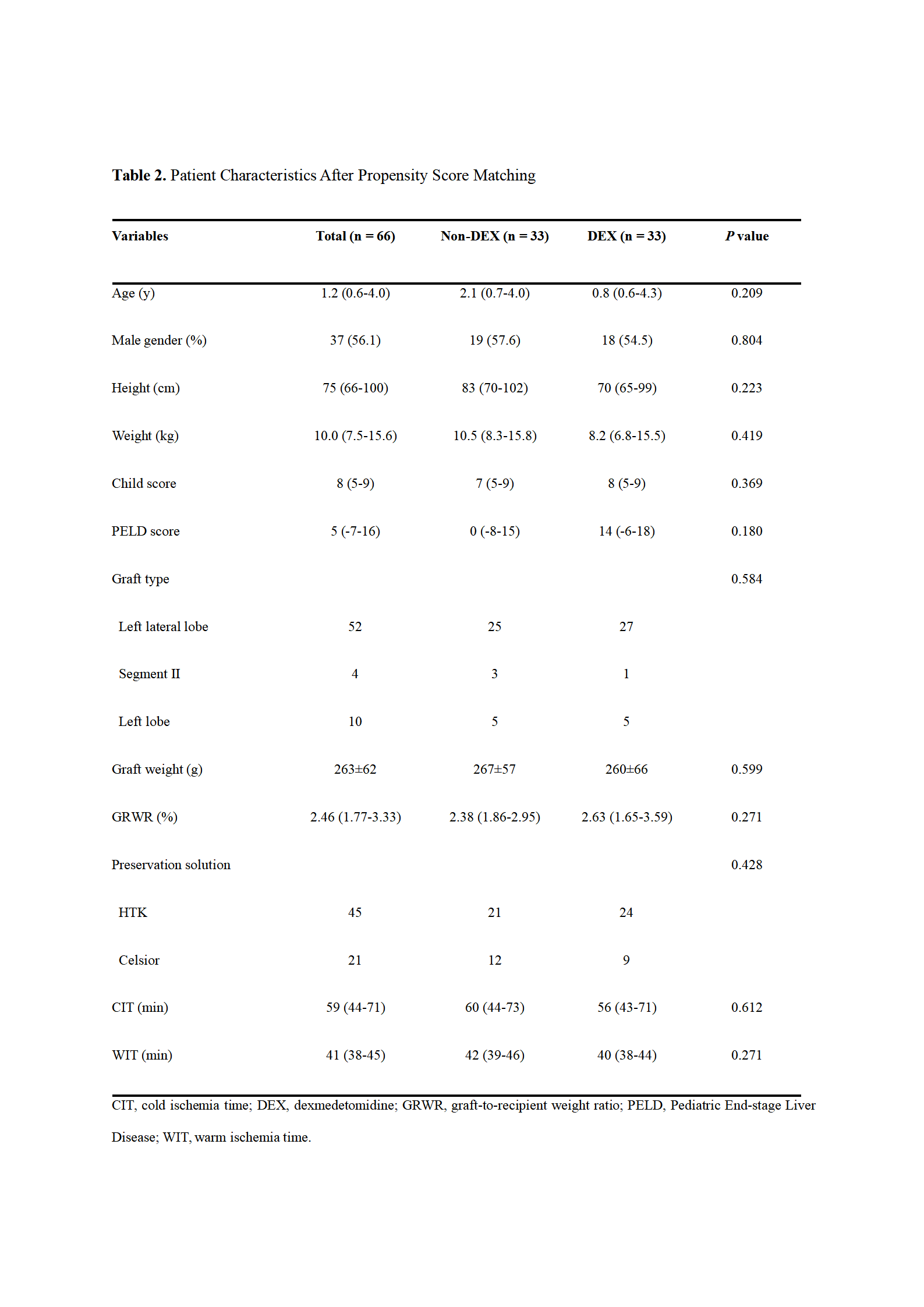
Even after PS matching, intraoperative DEX infusion was associated with decreased postoperative lactic dehydrogenase level and hospitalization (P = .047 and P = .020, respectively).
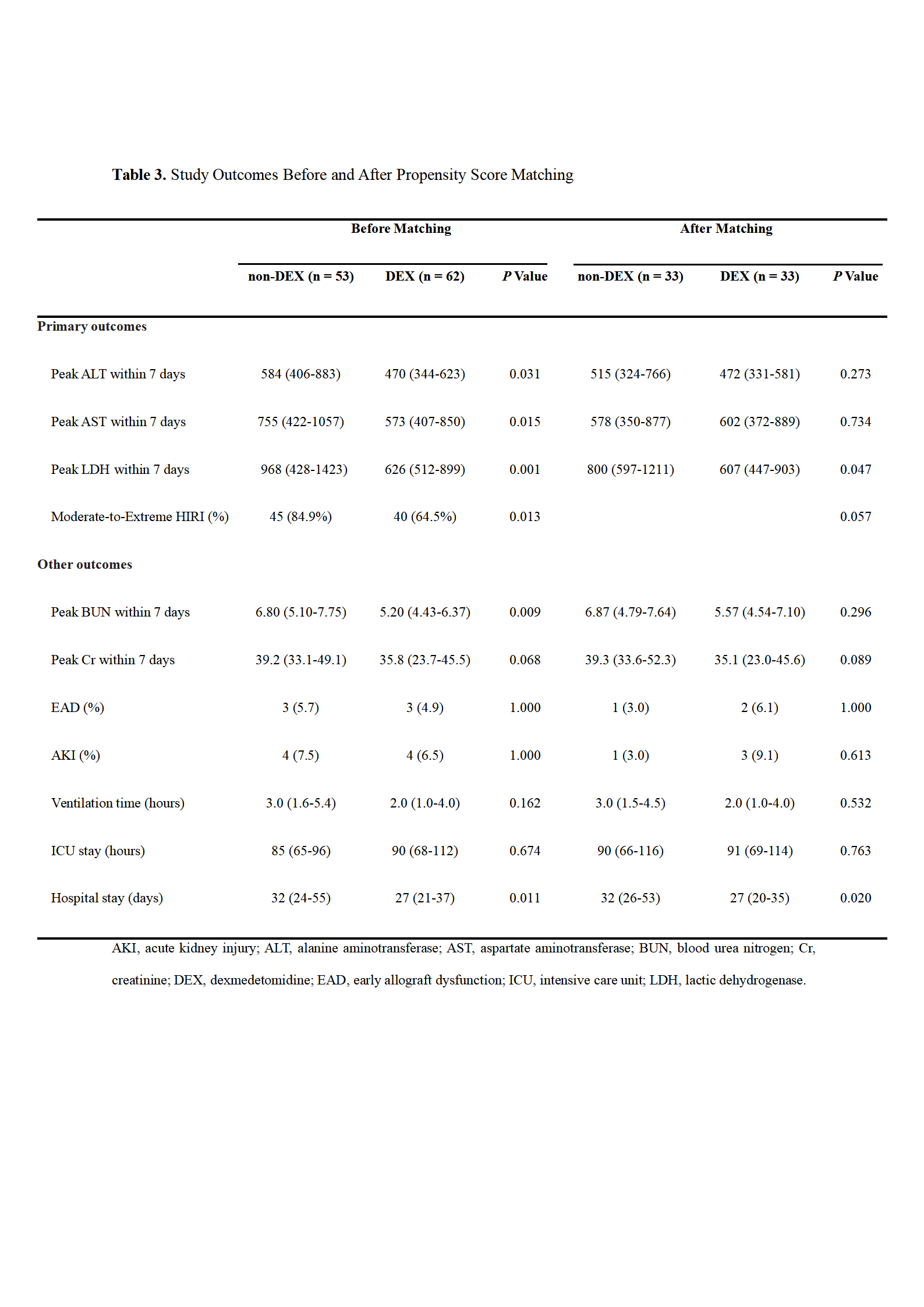
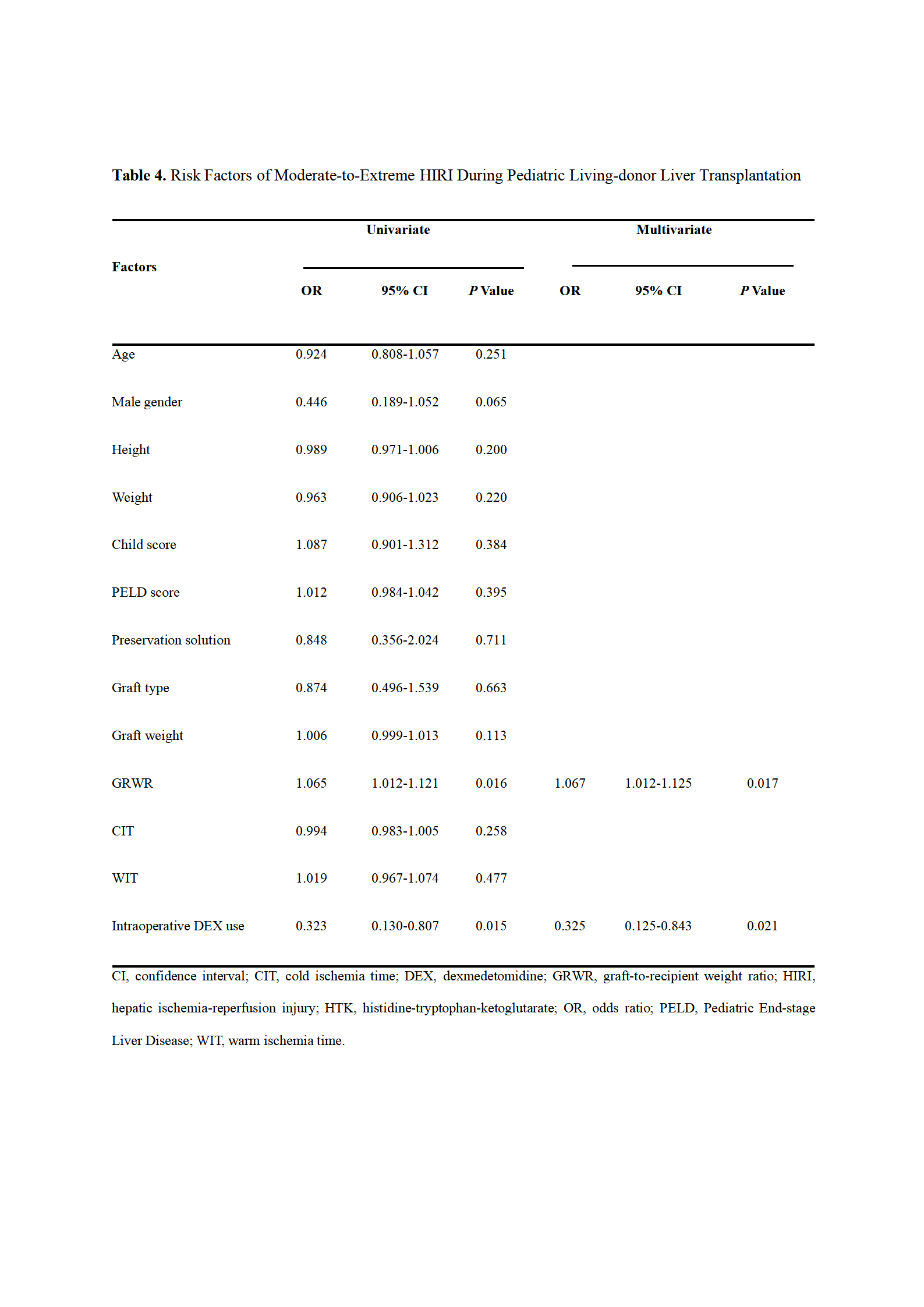
Moreover, multivariate analysis revealed that larger graft-to-recipient weight ratio (odds ratio [OR] = 1.067 [95% confidence interval {CI}, 1.012–1.125]; P = .017) and intraoperative DEX administration (OR = 0.325 [95% CI, 0.125–0.843]; P = .021) were independent predictors of moderate-to-extreme HIRI.
Conclusion: Intraoperative low-dose DEX infusion had a potentially protective effect liver graft function in pediatric LDLT without noticeably side effects.
[1] Friedman BH, Wolf JH, Wang L, Putt ME, Shaked A, Christie JD, Hancock WW, Olthoff KM. Serum cytokine profiles associated with early allograft dysfunction in patients undergoing liver transplantation. Liver Transpl. 2012; 18: 166-176.
[2] Nickkholgh A, Maluf D. Emerging graft protective strategies in clinical liver transplantation. Expert Rev Gastroenterol Hepatol. 2017; 11: 623-631.
[3] Zhai Y, Petrowsky H, Hong JC, Busuttil RW, Kupiec-Weglinski JW. Ischaemia-reperfusion injury in liver transplantation--from bench to bedside. Nat Rev Gastroenterol Hepatol. 2013; 11: 79-89.
[4] Sottas CE, Anderson BJ. Dexmedetomidine: the new all-in-one drug in paediatric anaesthesia? Curr Opin Anaesthesiol. 2017; 30: 441-451.
[5] Fayed NA, Sayed EI, Saleh SM, Ehsan NA, Elfert AY. Effect of dexmedetomidine on hepatic ischemia-reperfusion injury in the setting of adult living donor liver transplantation. Clin Transplant. 2016; 30: 470-482.
[6] Zhang L, Tian M, Xue F, Zhu Z. Diagnosis, Incidence, Predictors and Management of Postreperfusion Syndrome in Pediatric Deceased Donor Liver Transplantation: A Single-Center Study. Ann Transplant. 2018; 23: 334-344.
[7] Rosen HR, Martin P, Goss J, Donovan J, Melinek J, Rudich S, Imagawa DK, Kinkhabwala M, Seu P, Busuttil RW, Shackleton CR. Significance of early aminotransferase elevation after liver transplantation. Transplantation. 1998; 65: 68-72.
[8] Olthoff KM, Kulik L, Samstein B, Kaminski M, Abecassis M, Emond J, Shaked A, Christie JD. Validation of a current definition of early allograft dysfunction in liver transplant recipients and analysis of risk factors. Liver Transpl. 2010; 16: 943-949.
[9] Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO clinical practice guidelines for acute kidney injury. Kidney Int Suppl. 2012; 2(Suppl 1): 1-138.
[10] Tokodai K, Lannsjö C, Kjaernet F, Romano A, Januszkiewicz A, Ericzon BG, Nowak G. Association of post-reperfusion syndrome and ischemia-reperfusion injury with acute kidney injury after liver transplantation. Acta Anaesthesiol Scand. 2020; Feb 5 [Epub ahead of print].
[11] Guan L, Liu H, Fu P, Li Z, Li P, Xie L, Xin M, Wang Z, Li W. The Protective Effects of Trypsin Inhibitor on Hepatic Ischemia-Reperfusion Injury and Liver Graft Survival. Oxid Med Cell Longev. 2016; 2016: 1429835.
[12] Pratschke S, Angele MK, Grützner U, Tufman A, Bilzer M, Loehe F, Jauch KW, Schauer RJ. GSH attenuates organ injury and improves function after transplantation of fatty livers. Eur Surg Res. 2010; 45: 13-19.
[13] Zhang L, Tian M, Sun L, Zhu Z. Association Between Flushed Fluid Potassium Concentration and Severe Postreperfusion Syndrome in Deceased Donor Liver Transplantation. Med Sci Monit. 2017; 23: 5158-5167.
[14] Patrono D, Romagnoli R. Postreperfusion syndrome, hyperkalemia and machine perfusion in liver transplantation. Transl Gastroenterol Hepatol. 2019; 4: 68.
[15] Ito T, Nakamura K, Kageyama S, Korayem IM, Hirao H, Kadono K, Aziz J, Younan S, DiNorcia J 3rd, Agopian VG, Yersiz H, Farmer DG, Busuttil RW, Kupiec-Weglinski JW, Kaldas FM. Impact of Rifaximin Therapy on Ischemia/Reperfusion Injury in Liver Transplantation: A Propensity Score-Matched Analysis. Liver Transpl. 2019; 25: 1778-1789.
[16] Bharathan VK, Chandran B, Gopalakrishnan U, Varghese CT, Menon RN, Balakrishnan D, Sudheer OV, Dhar P, Surendran S. Perioperative prostaglandin e1 infusion in living donor liver transplantation: A double-blind, placebo-controlled randomized trial. Liver Transpl. 2016; 22: 1067-1074.
[17] Thies JC, Teklote J, Clauer U, Töx U, Klar E, Hofmann WJ, Herfarth C, Otto G. The efficacy of N-acetylcysteine as a hepatoprotective agent in liver transplantation. Transpl Int. 1998; 11 Suppl 1: S390-392.
[18] Hilmi IA, Peng Z, Planinsic RM, Damian D, Dai F, Tyurina YY, Kagan VE, Kellum JA. N-acetylcysteine does not prevent hepatorenal ischaemia-reperfusion injury in patients undergoing orthotopic liver transplantation. Nephrol Dial Transplant. 2010; 25: 2328-2333.
[19] Schauer RJ, Kalmuk S, Gerbes AL, Leiderer R, Meissner H, Schildberg FW, Messmer K, Bilzer M. Intravenous administration of glutathione protects parenchymal and non-parenchymal liver cells against reperfusion injury following rat liver transplantation. World J Gastroenterol. 2004; 10: 864-870.
[20] Gong Z, Ma L, Zhong YL, Li J, Lv J, Xie YB. Myocardial protective effects of dexmedetomidine in patients undergoing cardiac surgery: A meta-analysis and systematic review. Exp Ther Med. 2017; 13: 2355-2361.
[21] Jiang L, Li L, Shen J, Qi Z, Guo L. Effect of dexmedetomidine on lung ischemia‑reperfusion injury. Mol Med Rep. 2014; 9: 419-426.
[22] Jiang L, Hu M, Lu Y, Cao Y, Chang Y, Dai Z. The protective effects of dexmedetomidine on ischemic brain injury: A meta-analysis. J Clin Anesth. 2017; 40: 25-32.
[23] Bellos I, Iliopoulos DC, Perrea DN. Pharmacological interventions for the prevention of acute kidney injury after pediatric cardiac surgery: a network meta-analysis. Clin Exp Nephrol. 2019; 23: 782-791.
[24] Soleimanpour H, Nia KS, Sanaie S, Ghojazadeh M, Alavian SM. Use of Dexmedetomidine in Liver Disease: A Systematic Review and Meta-Analysis. Hepat Mon. 2019; 19: e98530.
[25] Rahman S, Davidson BR, Mallett SV. Early acute kidney injury after liver transplantation: Predisposing factors and clinical implications. World J Hepatol. 2017; 9: 823-832.
There are no comments yet...