Eliminating patient controlled analgesia reduces opioid use in renal transplant recipients
Marisa Schwab1, Hillary J. Braun1, Ryutaro Hirose1, Nancy L. Ascher1.
1Department of Transplant Surgery, University of California San Francisco, San Francisco, CA, United States
Introduction: Six percent of opioid-naïve patients develop opioid dependence post-operatively. Renal transplant recipients who fill opioid prescriptions for more than 90 days post-operatively are at increased risk for graft failure and death. We implemented a protocol in our renal transplant recipients that eliminated opioid patient-controlled analgesia (PCA) and included a multi-modal non-opioid regimen. The purpose of this study was to examine the impact of PCA elimination on opioid requirements at discharge in renal transplant recipients.
Materials and Methods: We reviewed adult renal transplant recipients for the three months prior to, and following, implementation of the protocol. Patients with an intra-abdominal transplant, a simultaneous pancreas-renal transplant, or a history of chronic pain were excluded. The number of opioid pills prescribed on the day prior to discharge were categorized as A) 0, B) 1-3, and C) 4. Discharge opioid prescriptions were then evaluated based on a recent recommendation that group A receive 0 pills, group B 15 pills, and group C 30 pills, to satisfy the outpatient pain needs of 85% of patients. Pre- and post- metrics were compared using independent t-tests and Chi squared tests.
Results and Discussion: 150 recipients were included (79 pre-intervention, 71 post; 51% male). 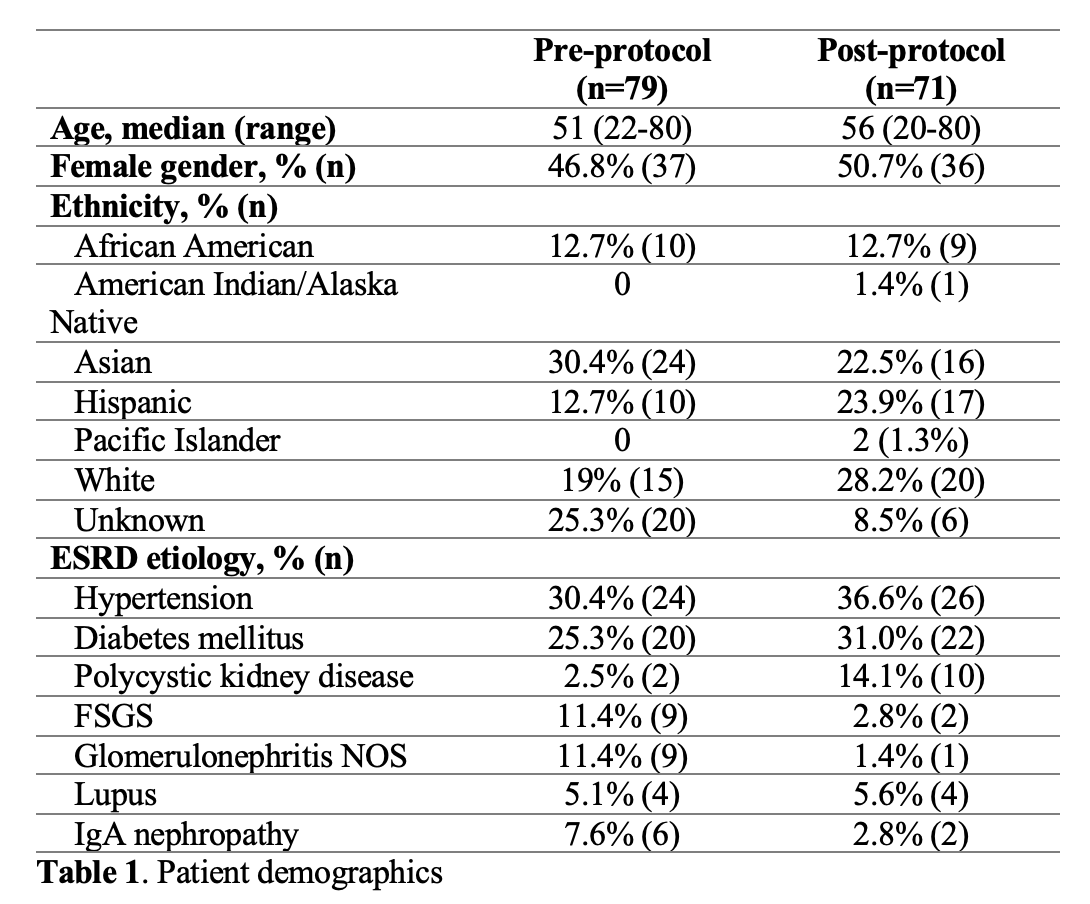 PCA use decreased significantly (95.8% vs. 19%, p<0.001). PCAs were associated with increased OMEs prescribed at discharge (84.3 vs. 68.5, p=0.14). Post-intervention, gabapentin, topical lidocaine, and acetaminophen increased significantly (7% to 73%, 6% to 68%, 72% to 94%, respectively)
PCA use decreased significantly (95.8% vs. 19%, p<0.001). PCAs were associated with increased OMEs prescribed at discharge (84.3 vs. 68.5, p=0.14). Post-intervention, gabapentin, topical lidocaine, and acetaminophen increased significantly (7% to 73%, 6% to 68%, 72% to 94%, respectively) 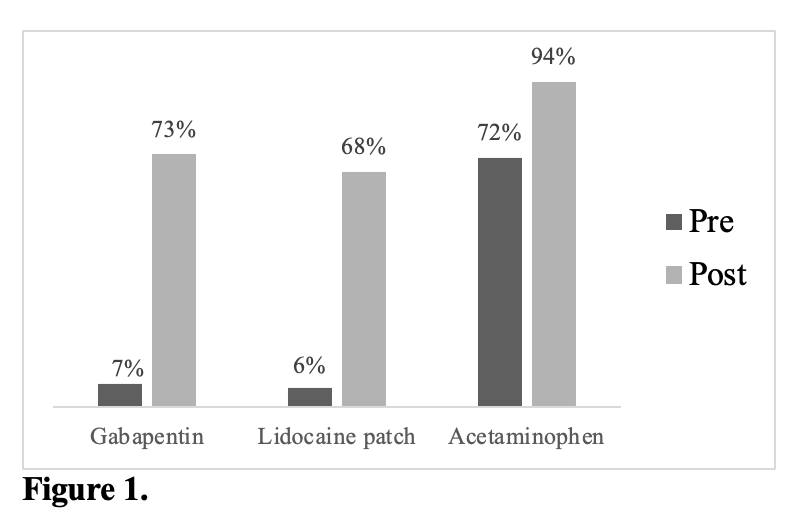 Of patients requiring no opioids on the day prior to discharge, 51.5% of pre- and 35.5% of post- were prescribed excess opioids at discharge.
Of patients requiring no opioids on the day prior to discharge, 51.5% of pre- and 35.5% of post- were prescribed excess opioids at discharge. 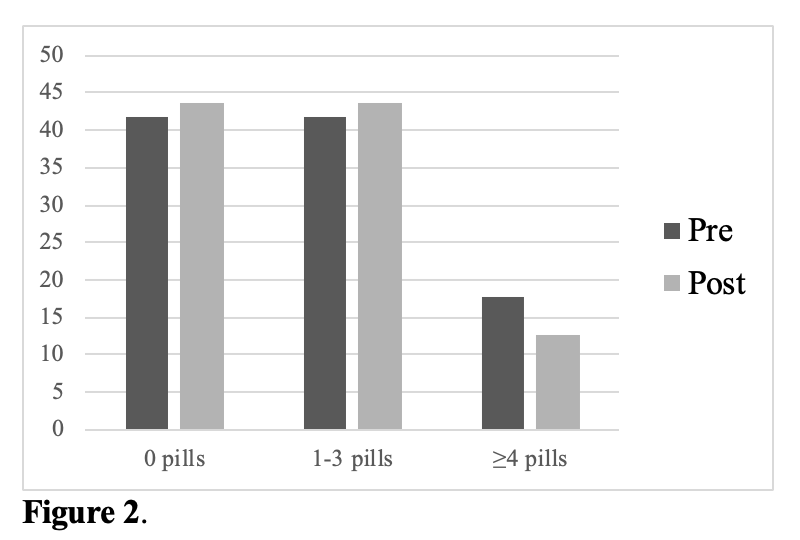 Of patients prescribed 1-3 pills on the day prior to discharge, 24.2% of pre- and 25.8% of post patients were prescribed excessive opioids at discharge.
Of patients prescribed 1-3 pills on the day prior to discharge, 24.2% of pre- and 25.8% of post patients were prescribed excessive opioids at discharge. 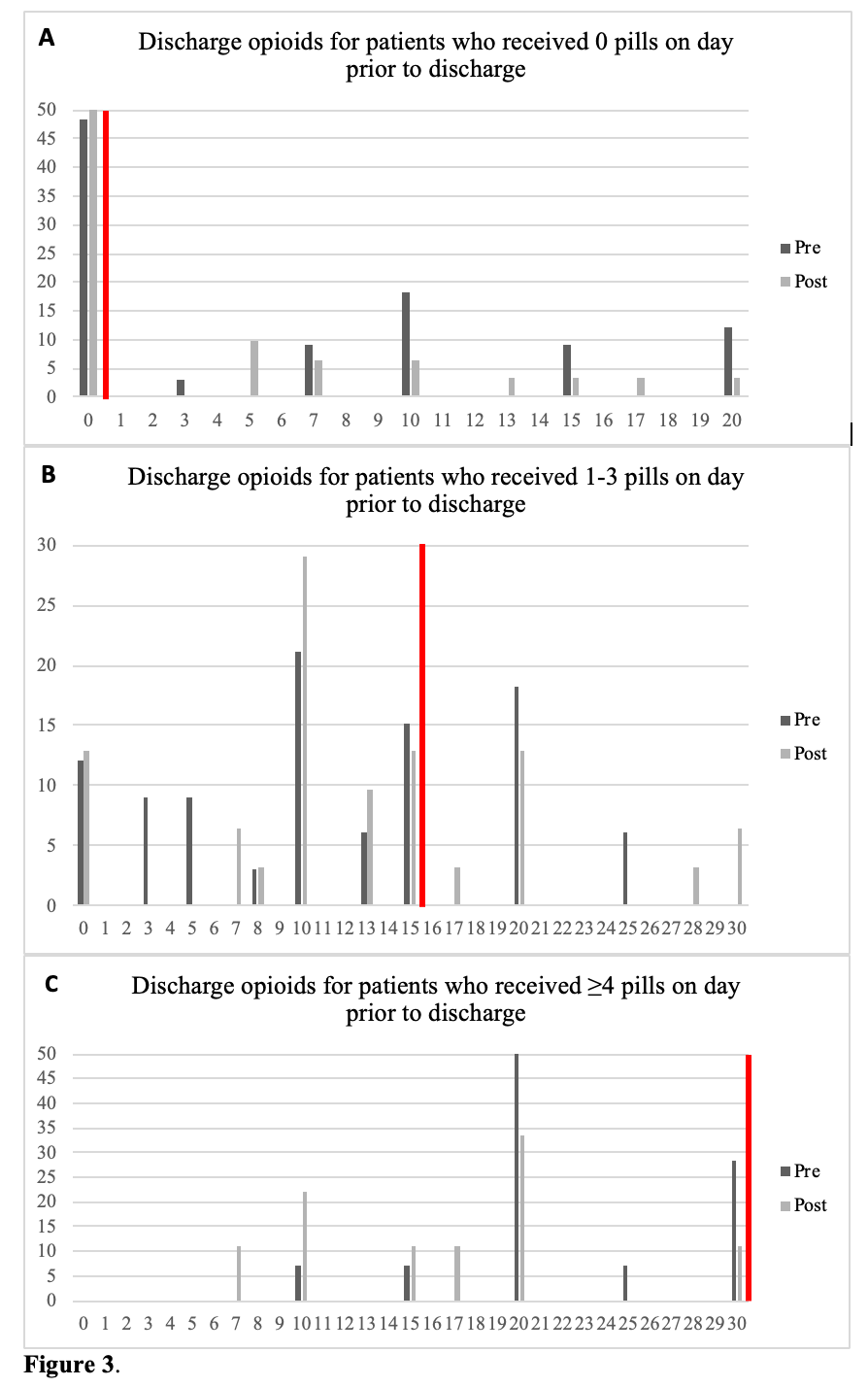
Conclusion: A multidisciplinary approach to developing an opioid-reducing protocol significantly decreased the use of PCAs and increased the use of non-opioid adjunct medications in renal transplant recipients. Eliminating PCAs trended towards a decreased amount of opioids prescribed at discharge. Excess opioids at discharge remains a problem. While we implemented a systems-based intervention to eliminate inpatient PCA prescription, we failed to adequately communicate the ultimate goal of decreasing opioids prescribed at discharge. Changing prescriber behavior requires specific interventions targeting all the metrics of interest. Following this study, we sought to protocolize both inpatient and discharge opioid prescribing wherein all patients, regardless of how many opioids received while inpatient, receive 10 opioid pills at discharge. After a three-month pilot, we plan to analyze the number of refills needed to evaluate whether this opioid-sparing approach at discharge leads to sufficient pain control in the short post-operative term.
Transplant surgery nursing staff, pharmacists, and clinical providers.
Ivonne Segura Nolasco
2020-09-13 18:48
Excelente trabajo muy buen aporte Felicitaciones