Impact of non-active hepatitis B on patient survival after renal transplantation
Marcel Naik1, Wiebke Duettmann1, Manuel Mayrdorfer1, Fabian Halleck1, Lukas Lehner1, Klemens Budde1, Michael Duerr1.
1Medical Department, Division of Nephrology and Internal Intensive Care Medicine, Charite, Berlin, Germany
Background: Incidence of hepatitis B (HB) infection is more frequent in end-stage renal disease patients (pts). After kidney transplantation (Ktx) chronic HB infection alone lead to significant inferior pts and graft survival. However, the majority of pts can resolve acute HB infection by clearing the surface antigen (HBsAg) and developing HB core antibodies. This so called non active HB pts is of utmost interest in terms of graft and pts survival in comparison to chronic active HBsAg positive infected KTx pts.
Methods: In our retrospective analysis we included all pts who received KTx from 01.01.1990 to 31.08.2019 in our center. In total, n=3663 were screened for HBsAg and for anti-HB core antibodies (HBcAb) prior to transplantation, defined by 180 days before and up to 20 days after KTx. Pts were categorized by serostatus as HB “naïve” (negative for HBsAg and HBcAb); “non-active” (positive for HBcAb but negative HBsAg) and “chronic” (HBsAg positive). Endpoints of this study were pts and graft survival by using Kaplan-Meier analysis and log-rank test.
Results: In 2491 KTx pts, serologic markers for HB were retrievable. We identified n=2198 HB naïve, n=218 non-active HB and n=75 chronic HB pts. Overall 484 graft failures occurred (19.4%) and 672 patients (27%) died. Kaplan-Meier-analysis showed a 5-year graft survival of 87.7% in the naïve group, 86.0% in non-active HB and 85.4% in chronic HB group.
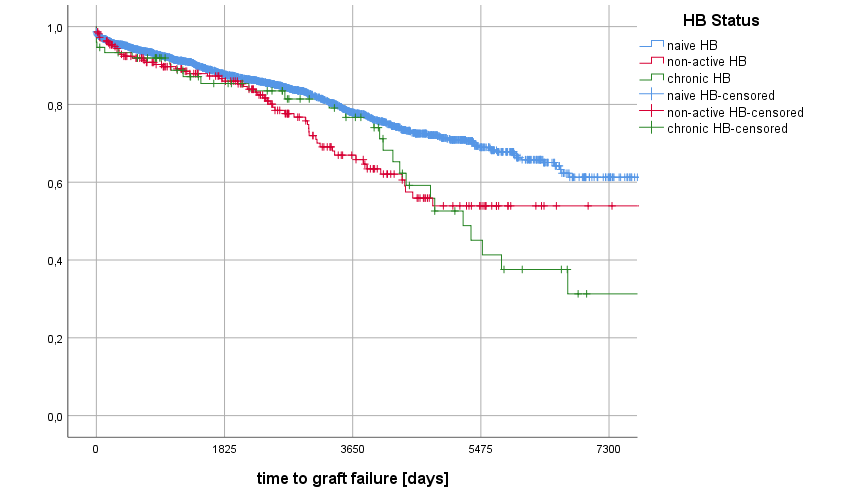
The 10-year-graft survival was 77.9% in naïve group, 66.9% in non-active HB and 76.7% in chronic HB group. The 20-year-graft survival was 61.3% in naïve group, 53.9% in non-active HB and 31.3% in chronic HB group (p=<0.001). Patient survival after 5 years was 87.5% in the naïve group, 83.7% in non-active HB group and 82.2% in chronic HB group.
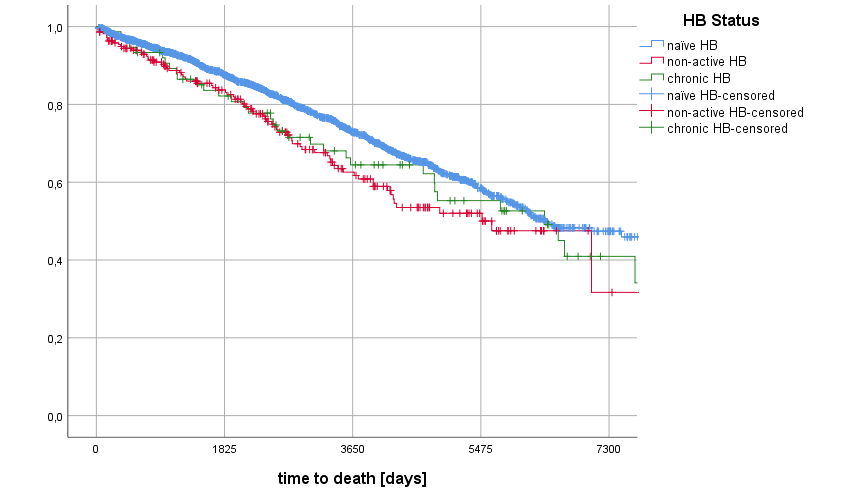
The 10-year-pts survival was 73.0% in the naïve group, 62.6% in non-active HB group and 64.5% in chronic HB group. The 20-year-ptx survival was 47.4% in naïve group, 31.7% in non-active HB and 40.9% in chronic HB group (p=0.013). Overall patient and graft survival after 5 years was 79.1% in the naïve group, 74.7% in non-active HB group 69.9% in chronic HB group.
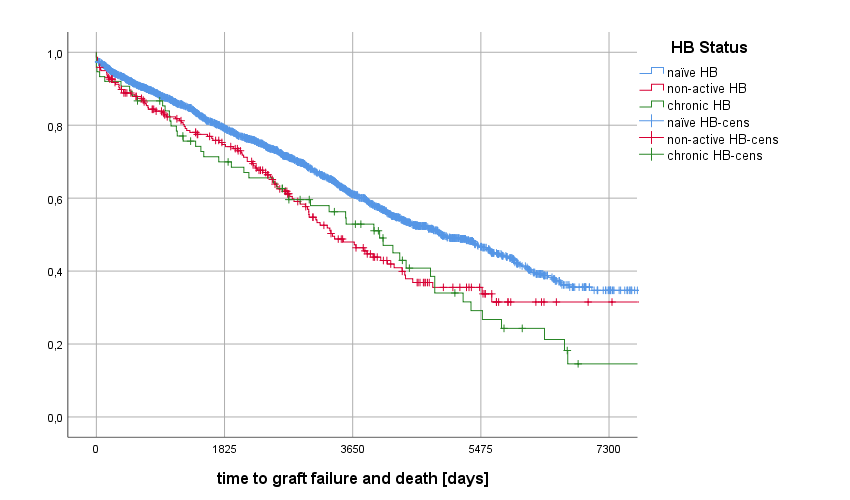
The 10-year-rate was 61.1% in the naïve group, 48.0% in non-active HB group and 52.2% in chronic HB group (p<0.001). The 20-year-overall survival was 34.7% in naïve group, 31.5% in non-active HB and 14.6% in chronic HB group (p<0.001).
Conclusions: Hepatitis B leads to earlier graft loss and inferior pts survival. Of note, beside already known negative effect of chronic HB infection, also in non-active infected HB pts overall survival was significant worse to HB naïve pts. Thus, non-active HB status is an important risk factor for overall transplant outcome. Further studies of occult HB virus replication could add substantial value to understand the negative impact of non-active HB. In a next stept we want to include the vaccination status and hepatitis antibody levels for further risk stratification.