1 -year protocol biopsies in pediatric kidney transplant children: Are unfavorable histological lesions related to no adherence?
Marta Lidia Monteverde1, Jennifer M. Velasco1, Veronica Solernieu2, Juan P. Ibanez1, Alicia B. Chaparro1, Cintia Y. Marcos4, Carolina Cernadas3.
1Nephrology, Hospital de Pediatria JP Garrahan, Ciudad Autónoma de Buenos Aires, Argentina; 2Pathology, Hospital de Pediatria JP Garrahan, Ciudad Autónoma de Buenos Aires, Argentina; 3Teaching and Research, Hospital de Pediatria JP Garrahan, Ciudad Autónoma de Buenos Aires, Argentina; 4Hemotherapy, Hospital de Pediatria JP Garrahan, Ciudad Autónoma de Buenos Aires, Argentina
Introduction: In adult recipients histological findings in surveillance biopsies at 1-year post kidney transplantation (KT) correlate independently with short and long-term graft survival. Donor specific antibodies (dnDSA) are associated with antibody- mediated rejection. Non-adherence (NOA) to treatment, is a risk factor for dnDSA. Studies in children with KT with protocol biopsies are scarce.
Objective: To evaluate the prevalence of favorable (FAV) and unfavorable (UNFAV) histological lesions (FAV) for graft survival in 1-year protocol biopsies of KT children and to identify risk variables for these lesions.
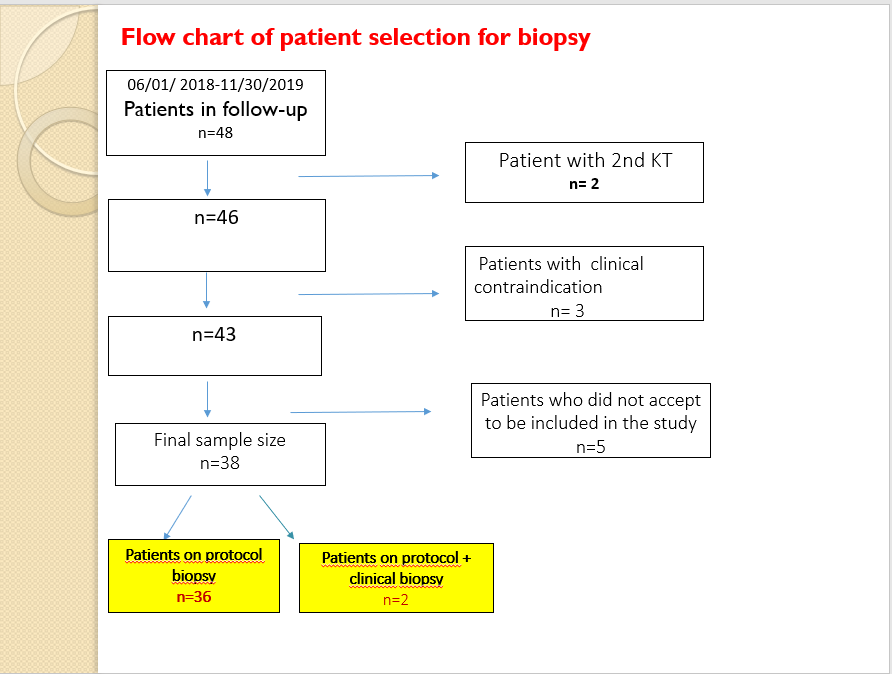
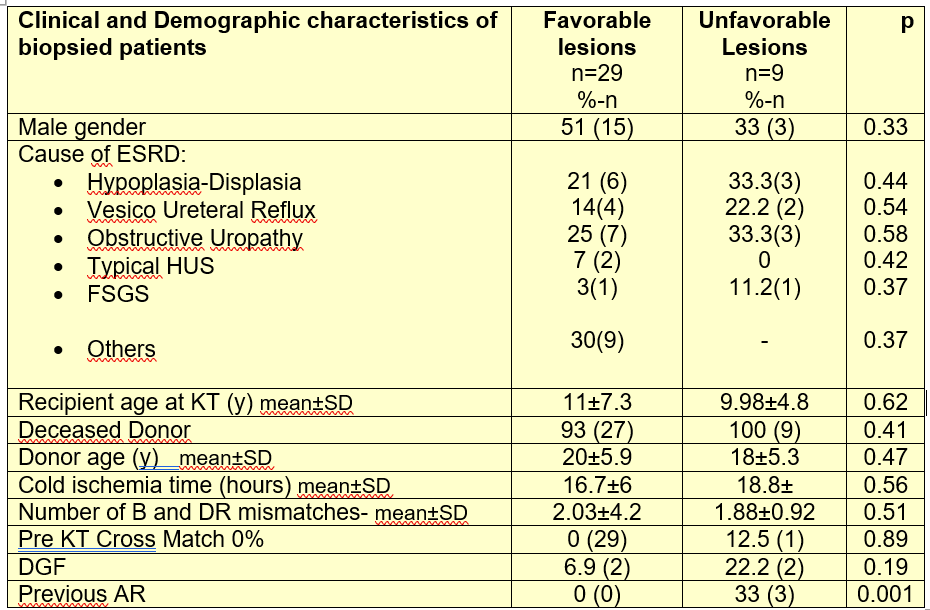
Methods: Prospective cohort study in all recipients of a 1st KT between 06/01/2018 and 05/30/2019. (TABLE 1) According to their histological risk, lesions were grouped in “FAV” and “UNFAV”. “FAV” lesions were: 1) minor morphological changes, with absence of inflammation and / or fibrosis and / or chronic glomerulopathy or glomerulonephritis, 2) Acute Interstitial inflammation without interstitial fibrosis or glomerular changes 3) Mild Interstitial fibrosis with absence of interstitial inflammation. “UNFAV” lesions were: 1) moderate-severe interstitial fibrosis without inflammation 2) acute or chronic active rejection mediated by antibodies or T cells 3) de novo glomerular disease 4) polyoma virus-associated nephropathy. dn-DSA were sought simultaneously with kidney biopsy. TAC and / or SRL variation coefficient (VC) >25% was considered a surrogate of NOA.
Results: 38 children were included. 29 had “FAV” lesions (76%): 23, Minimal morphological changes, and 6 mild fibrosis. Nine had “UNFAV” histology (24%): One had disease recurrence, three acute vascular rejection, (2/3 subclinical rejection; 1/3 DSA+) and four had moderate fibrosis (2 had graft hydronephrosis and 2 had previous AR,1DSA+). Mean eGFR in patients with “UNFAV” lesions was 39 ± 12.1 ml / min/ 1.73m2 vs 65.3 ± 18 ml / min / 1.73m2 in those with “FAV” (p=0.0003). Both groups had similar pre KT clinical and demographic characteristics. (TABLE2). UNFAV patients had higher incidence of previous Acute Rejection (TABLE2). TAC or SRL VC was: < 25% in 71% of patients (n= 27), and > 25% in 19% of patients (n=11), those with irregular intake. Children with VC> 25% had higher risk of an “UNFAV” lesion in protocol biopsy (OR: 4.8; p=0,04) and higher prevalence of dnDSA (18% vs 0%; p=0.02)
Conclusion: In this cohort, FAV lesions were the most prevalent and were associated with negative dnDSA and TAC or SRL VC <25%. Children with UNFAV lesions had lower eGFR. Those with TAC or SRL VC>25% had higher risk of an “UNFAV” lesion, and higher prevalence of dnDSA. Follow-up of this cohort is imperative.
[1] F.G Cosio et al. American Journal of Transplantation 2016; 16: 194–203
[2] Maritere Nazario et al. Pediatric Transplantation. 2018;22:e13178. Pediatric Transplantation. 2018;22:e13178.
[3] David N. Rush, and Ian W. Gibson. Transplantation 2019;103:e139–e145
There are no comments yet...
