
Single centre experience on ultra low dose Thymoglobulin as an induction agent in low immunological risk living kidney transplant recipients
Maisarah Jalalonmuhali1, Kok Peng Ng1, Albert Hing Wong1, Yee Wan Lee1, Chye Chung Gan1, Chew Ming Wong1, Wan Ahmad Hafiz Wan Md Adnan1, Soo Kun Lim1.
1Division of Nephrology, Department of Medicine, University Malaya Medical Centre, Kuala Lumpur, Malaysia
Background: Significant advancement in solid organ transplant immunosuppressive medications have resulted in improved graft outcome over the years. Polyclonal antibody [rabbit anti-thymocyte globulin (rATG) @ thymoglobulin)] used in induction regime is very potent with dose dependent effects. Thus the aim of this study is to look at the outcome of ultra-low dose thymoglobulin in low immunological risk kidney transplant recipients (KTR).
Methodology: This is a prospective randomized study recruiting all low immunological risk recipients. Low immunological risk defined as negative for CDC crossmatches for T and B cells as well as no detectable preformed HLA-DSA. The patients were given either basiliximab 20 mg on day-0 and day-4 or low dose thymoglobulin (0.5 mg per kilogram of body weight daily) on day-0, day-1 and day-2. Their renal function, HLA- donor specific antibodies (DSAs), lymphocyte counts, protocol biopsies and cytomegalovirus (CMV) polymerase chain reaction (PCR) were monitored as per clinical practice.
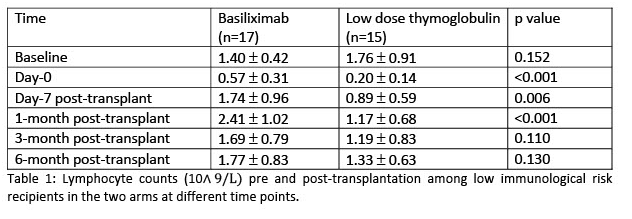
Results: A total of 32 patients were recruited in this study. Their mean age was 41.91 + 13.04 years old. 17 of the patients received basiliximab while another 15 had low dose thymoglobulin. All the patients in both arms had immediate graft function with mean serum creatinine of 110.27 + 32.27 at 3 months post transplantation and 110.07 + 26.75 at 6 months post transplantation in basiliximab group. While in low dose thymoglobulin group, their mean serum creatinine were 135.92 + 42.1 and 137.85 + 36.91 respectively at 3 months and 6 months post transplantation. However, there were no significant difference in the incidence of de novo HLA-DSA, CMV and BKV viraemia. Interestingly, the lymphocyte counts in low dose thymoglobulin group is significantly lower up until at 1 month post transplantation (table 1).
Conclusion: Very low dose thymoglobulin is non-inferior in comparison with current induction therapy in low risk recipients with more pronounced and sustained lymphocyte depletion in preventing early acute rejection.
There are no comments yet...
