A personalised prediction model for allograft survival after kidney transplantation
Yunwei Zhang1,2, Jean Yang1,2, Germaine Wong3,4,5,6, Samuel Mueller1.
1School of Mathematics and Statistics, Faculty of Science, The University of Sydney, Sydney, Australia; 2Charles Perkins Centre, The University of Sydney, Sydney, Australia; 3Sydney School of Public Health, The University of Sydney, Sydney, Australia; 4Centre for Kidney Research, Sydney, Australia; 5Kids Research Institute, Sydney, Australia; 6The Children’s Hospital at Westmead, Sydney, Australia
Introduction: Identification of novel risk factors for adverse allograft outcomes will allow prevention and early intervention before detrimental events arise. We aimed to develop a robust, validated, personalised prediction model for long-term allograft survival in deceased donor kidney transplant recipients.
Materials and Methods: We develop a novel approach using unsupervised learning algorithm and penalised cox model with data from the Australian and New Zealand dialysis and transplant registry (ANZDATA, 2006 – 2017). We used Numero to cluster groups of recipients based on their non-immunological characteristics. Numero is an unsupervised learning approach based on Self-organising maps (SOM) which is specially designed to characterise variability and summarise key features in a cohort dataset. We then applied Elastic net cox model (a penalised cox model) to identify the baseline recipients and donor risk factors associated with the allograft survival.
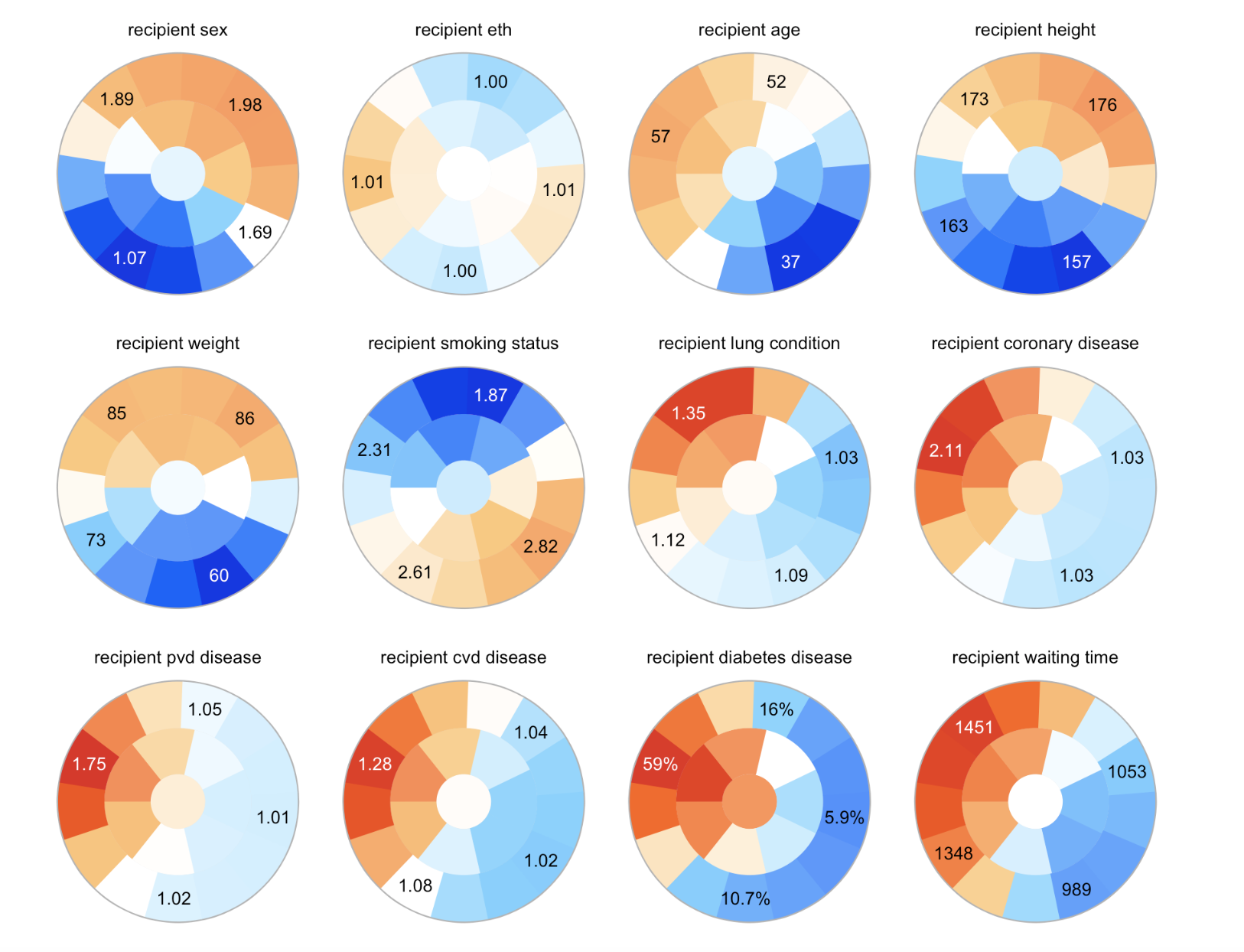
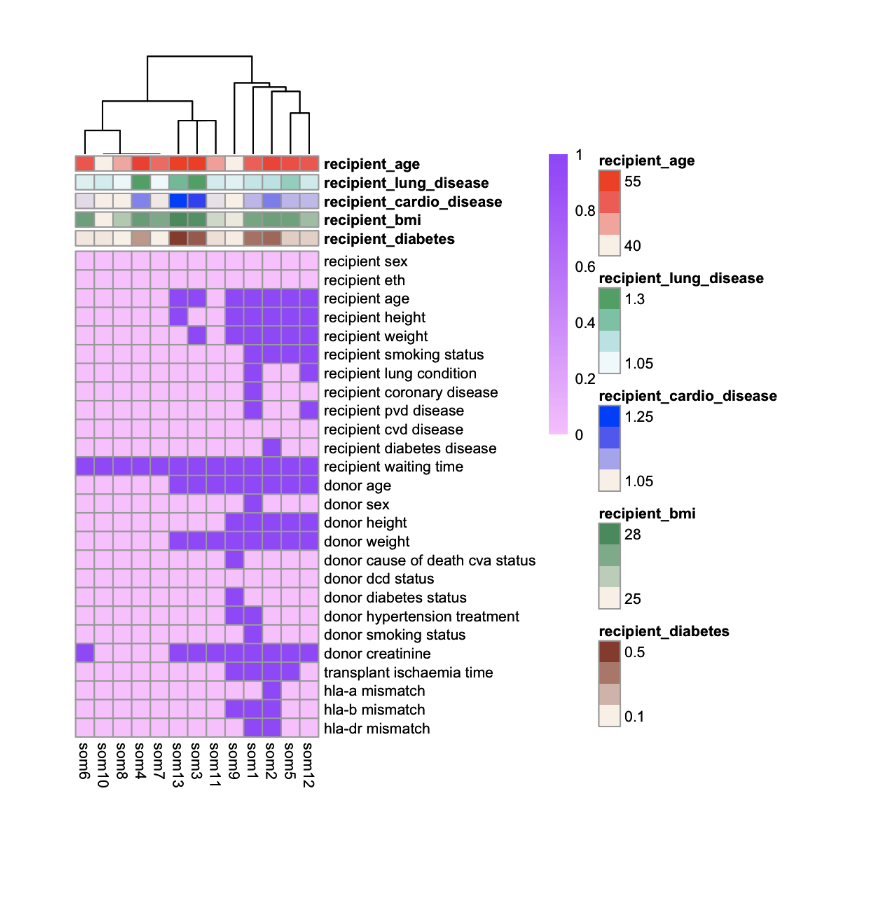
Results: A of 3692 deceased donor kidney transplant recipients were included in the study. Clustering with Numero generated 13 groups with different recipients’ baseline characteristics. We then further divided the cohort into three clusters using the Elastic cox model. These were classified as 1) recipients with no significant comorbid disease, 2) recipients with some comorbid illness and 3) older recipients with multiple comorbid diseases. The key factor most strongly predicted allograft survival across these three subgroups was waiting time on dialysis. Other immunological factors such as HLA A, B and DR mismatches and non-immunological disease related factors were only predictive of allograft survival in recipients’ multiple comorbidities. The overall c-index of the predictive modelling was 0.69.
Conclusion: Waiting time on dialysis is the key risk factor for long-term allograft survival across the entire cohort. However, the impact of immunological and non-immunological factors for the prediction of allograft survival is most marked among those with multiple comorbidities.