Parameters affecting estimated glomerular filtration rate and developing hypertension after donor nephrectomy
Zeynep Kendi Celebi1, Didem Turgut1, Cihad Burak Sayin1, Turhan Colak1, Mahir Kirnap2, Mehmet A. Haberal2.
1Nephrology, Baskent University, Ankara, Turkey; 2Transplantation, Baskent University, Ankara, Turkey
Introduction: Kidney transplantation is the choice of treatment for renal replacement therapy in patients with end stage renal disease(ESRD). The evaluation of kidney donor and recipients are focused on protecting the donor from future diseases and ensuring maximum graft survival in the recipient.
In this study, we aimed to evaluate the effects of predonation factors on developing hypertension(HT) and the estimated glomerular filtration rate(eGFR) at the follow-up in living kidney donors.
Method: Total 1059 kidney donor was evaluated, who donated a kidney between 1997 and 2019 at Başkent University. Of these patients, who had at least 1 year after nephrectomy and who were followed-up in our hospital were included in the study.
The predonation- 1 months after donation and the last follow up parameters including biochemical parameters, blood pressure levels and diabetes mellitus(DM), HT, atherosclerotic heart disease(AHD) were recorded. The SPSS 22.0 was used for statistical analysis and p<0.05 was considered to be significant.
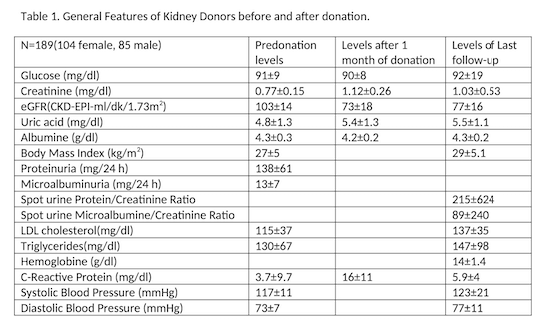
Results: 189 patients were included to the study.Mean age of donors was 50±11 years, age at donation was 43±10 years and follow up time was 89±64 months. General features of patients at predonation, at first month after donation and at the last follow up were given in Table 1.
At follow-up, 22 donors had DM(11.6%), 13 donors had AHD(6.9%), 52 donors had hyperlipidemia (27.5%), 54 donors had HT(28.6%) and 21 of these 54 patients diagnosed at the last follow-up with HT. When smoking status assesed 55 donors were active smoker and 15 donors were ex-smoker.
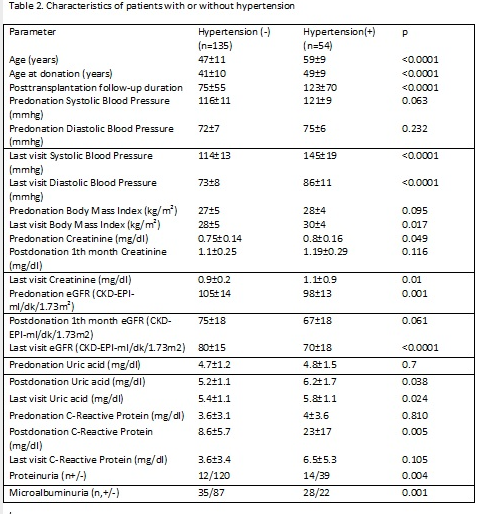
The characteristics of patients with and without HT are given in Table 2. DM, hyperlipidemia, AHD were observed more frequently and smoking amount was higher in patients with HT (p<0.0001). Regression analysis showed that age at donation was the independent risk factor for developing HT (p=0.034 OR=1.088, 95% CI= 1.006-1.177).
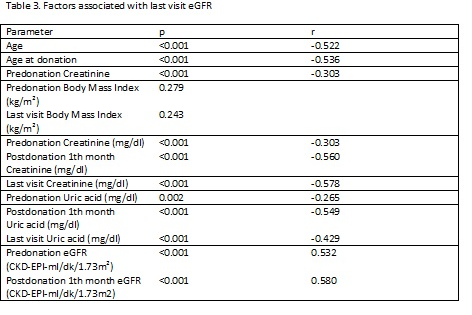
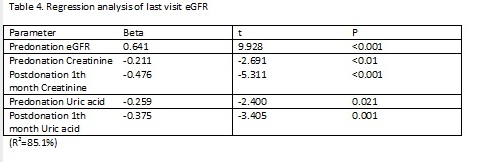
Our donors develop approximate 30 ml/min/1.73m2 eGFR decline after nephrectomy and than an increase 4 ml/min/1.73m2 after compensation. The parameters associated with last visit eGFR were given in Table 3. Regression analysis for last visit eGFR is given in Table 4.
Conclusion: Our study showed that, almost 30% of donors had developed hypertension. Age at donation is the main risk factor for developing HT after kidney donation. Postdonation eGFR level is associated with predonation eGFR levels positively and both pre and postdonation creatinine and uric acid levels negatively. Donors should be closely followed-up for development of hypertension and chronic kidney disease.