Analyzing causes for death-censored allograft failure in kidney transplant recipients
Manuel Mayrdorfer1, Lutz Liefeldt1, Nils Lachmann2, Wiebke Düttmann-Rehnolt1, Marcel Naik1, Petra Glander1, Fabian Halleck1, Klemens Budde1.
1Department of Nephrology, Charité University Medicine Berlin, Berlin, Germany; 2HLA Laboratory, Center for Tumor Medicine, Charité University Medicine Berlin, Berlin, Germany
Introduction: Since it has been proposed that several causes could contribute to graft loss (GL), we analyzed graft failure in our center and attributed a cause to each persistent decline in renal function, finally leading to GL.
Materials and Methods: We retrospectively analyzed 1412 recipients of a renal allograft, transplanted between 01.01.1997 and 31.12.2016 in a single center, of which 290 progressed to GL. An adjudication committee consisting of 3 physicians, 2 of which have personal knowledge of recipients for over 20 years, evaluated indication biopsies, laboratory testing and medical history. Non-reversible decreases in glomerular filtration rate were attributed to primary and/or secondary causes.
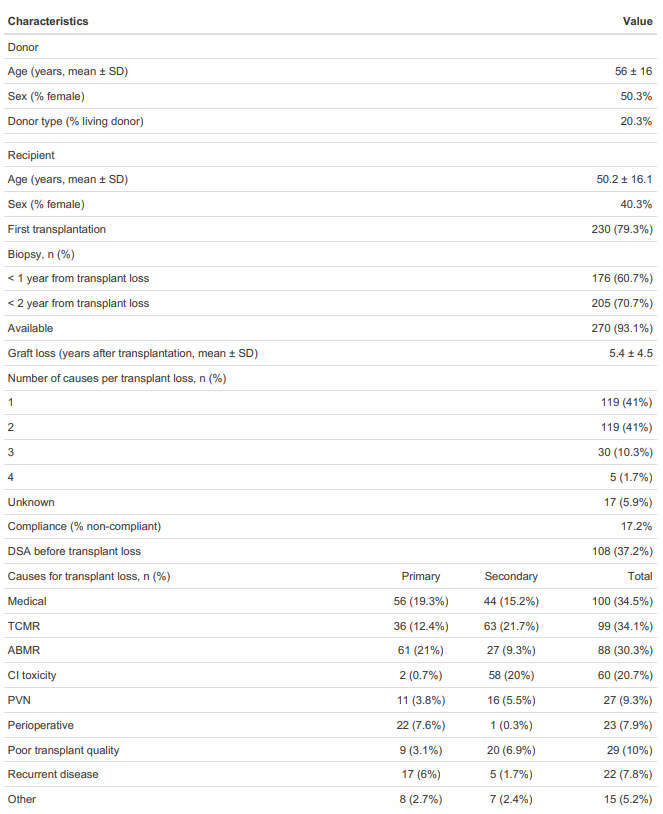
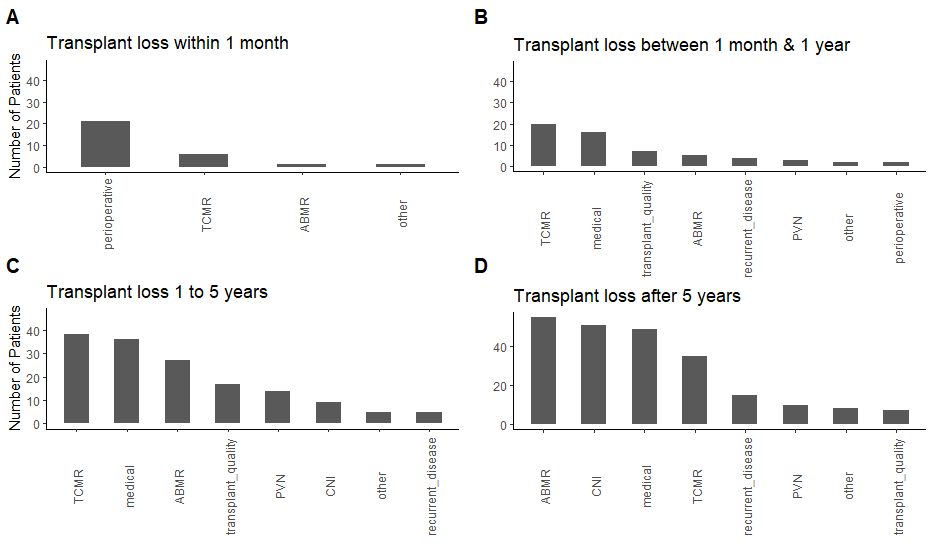
Results and Discussion: Characteristics of patients who progressed to GL are summarized in table 1. In 53.1% of the patients, more than one cause contributed to GL. The most frequent cause leading to GL as primary or secondary cause were intercurrent medical events in 34.5% of the patients, followed by T cell mediated rejection (TCMR) in 34.1% and antibody-mediated rejection (ABMR) in 30.3%. In 76.6% a primary cause could be attributed to transplant loss, of which 27.5% were ABMR. Moreover, we observed a shift in overall causes with regard to the timing of GL, in the form of an increasing relative frequency of ABMR and calcineurin inhibitor (CNI) nephrotoxicity (figure 1). Taking into account only primary causes, the dominant role of ABMR in late GL becomes more and more evident (figure 2).
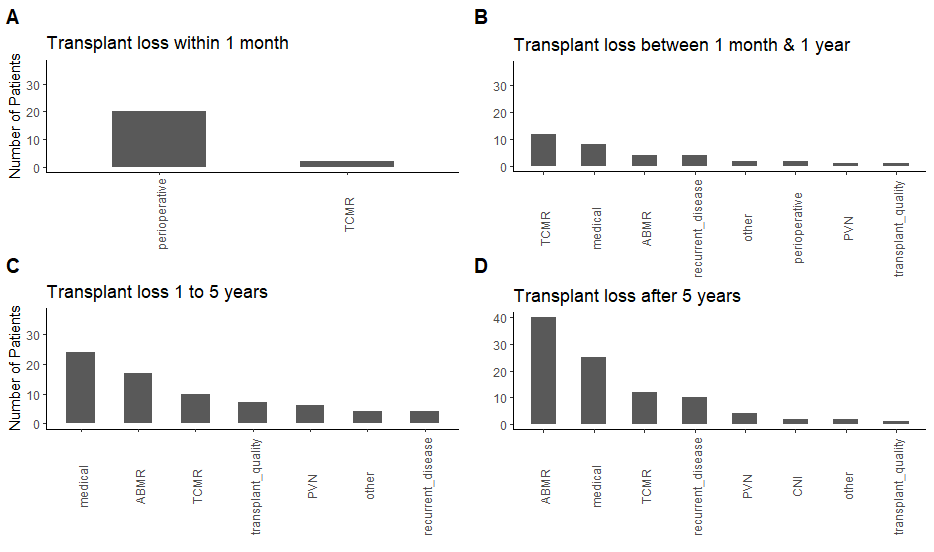
Conclusion: Analyzing all graft failures in a long-term follow-up cohort of 290 patients, we observed that >50% of failures were multifactorial. Our results show a significant role of TCMR in graft failure that would be dismissed in most of the cases focusing just on the final stage of graft failure. Additionally, we were able to attribute an intercurrent medical event to GL in 34.5% of the patients and to highlight the dominant role of ABMR in late graft failure.
