Enhanced functional recovery of hearts donated after circulatory death (DCD) with ante-mortem heparin.
Ling Gao1, Aoife Doyle1, Jeanette Villanueva1, Sarah Scheuer1,3, Hong Chew1,3, Mark Hicks1,2, Peter SS Macdonald1,3.
1Cardiac Physiology and Transplantation, Victor Chang Cardiac Research Institute, Sydney, Australia; 2Department of Clinical Pharmacology & Toxicology, St Vincent’s Hospital, Sydney, Australia; 3Heart & Lung Transplant Unit, St Vincent’s Hospital, Sydney, Australia
Background: DCD hearts are now an important source for transplantation [1]. Among unknowns during DCD organ retrieval is the need for ante-mortem heparin which is currently not permitted in some jurisdictions due to ethical concerns. While administration of ante-mortem heparin has been shown experimentally to improve perfusion of abdominal organs during regional perfusion after withdraw of life support (WLS) [2], the impact of ante-mortem heparin on the recovery of cardiac function following retrieval from DCD donor has not been reported. In a recent analysis of clinical outcomes of DCD heart transplantation in our program, we found that the asystolic warm ischemic time (aWIT) between circulatory arrest and the commencement of cold flush of the heart was critical to the early outcome of the donor heart after implantation [3]. Here, in a DCD model designed to mimic this clinical scenario, we aimed to investigate: 1) the susceptibility of DCD hearts to increasing aWIT; 2) the impact of ante-mortem heparin administration on recovery of DCD heart during normothermic ex situ reperfusion.
Methods: Male Wistar rats (340-420g) were anesthetized and carotid artery was cannulated for blood pressure monitoring. WLS was initiated by tracheal ligation with or without ante-mortem injection of 500 IU heparin. Circulatory arrest was declared when pulse pressure trace disappeared. Animals were randomized into experimental groups exposed to increasing aWIT of 10, 15 and 20 min. After each aWIT period, hearts were excised then flushed with 100 ml ice-cold Celsior followed by 1 hr reperfusion (30 min Langendorff, 30 min working mode) with Krebs solution at 37oC. Sham hearts were removed after heparin injection without tracheal ligation. Recovery of cardiac function after reperfusion was assessed by measurement of aortic flow (AF), pulse pressure (PP), heart rate (HR) and coronary flow (CF). Timed collection of coronary effluents during reperfusion were assessed for lactate dehydrogenase (LDH) and troponin-I (cTnI).
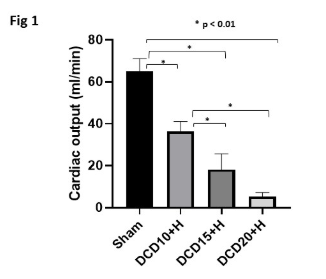
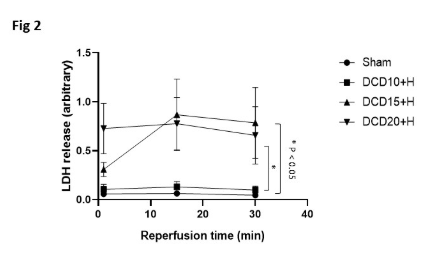
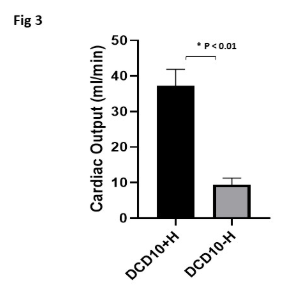
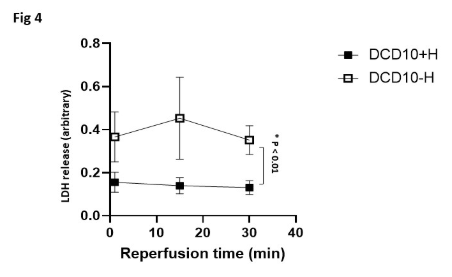
Results: All DCD hearts had significantly lower functional recoveries after reperfusion compared to sham controls. The recovery of DCD heart function was inversely proportional to the duration of aWIT (Fig1). LDH levels were significantly higher in 15 and 20 aWIT hearts (Fig2). When exposed to aWIT of 10min, hearts retrieved after ante-mortem heparin had significantly better functional recovery (Fig3) and reduced LDH (Fig4) and cTnI release compared to those without ante-mortem heparin.
Conclusions: This is the first study specifically investigating the impact of ante-mortem heparin on the recovery of DCD hearts after retrieval. We show ante-mortem heparin administration significantly enhanced recovery of DCD heart function, associated with reduced LDH and cTnI release. We believe that administration of ante-mortem heparin in DCD heart retrieval is beneficial and may improve donor heart quality with the potential to reduce risk of PGD post-implantation.
St Vincent’s Clinical Foundation of Australia (SVCF-PM). National Health & Medical Research Council of Australia (program grant ID 1074386).
[1] Chew HC, Iyer A, Connellan M, et al. Outcome of Donation after Circulatory Death Heart Transplantation in Australia. J Am Coll Cardio 2019; 73:1447– 59.
[2] Rojas-Pena A et al. Timing of Heparin and Perfusion Temperature During Procurement of Organs with Extracorporeal Support in Donors After Circulatory Determination of Death. ASAIO J 2011; 57: 368-74.
[3] Scheuer S.E et al. Getting the time right: what matters, what doesn’t, and how should we really be defining ischemic times in DCD withdrawals? Journal of Heart & Lung Transplantation; 2020, in press.
