Consent to organ offers from public health service “increased risk” donors decreases time to transplant and waitlist mortality
Yvonne Kelly1, Arya Zarinsefat1, Mehdi Tavakol1, Amy M. Shui1, Chiung-Yi Huang1, John Roberts1.
1Surgery, University of California, San Francisco, San Francisco, CA, United States
Introduction: The Public Health Service “Increased Risk” (PHS-IR) designation identifies organ donors who are at increased risk of transmitting hepatitis B, hepatitis C, and human immunodeficiency virus. Despite data showing these organs are safe for transplant with a risk of disease transmission ranging from 0.04-4.9/10,000, many patients and families are hesitant to consent to organ offers from donors in this category and studies have shown these organs are highly underutilized. We hypothesize that patients who do consent to organ offers from PHS-IR donors will have a decreased time to transplant and a decreased waitlist mortality compared to patients who do not consent to offers from PHS-IR donors.
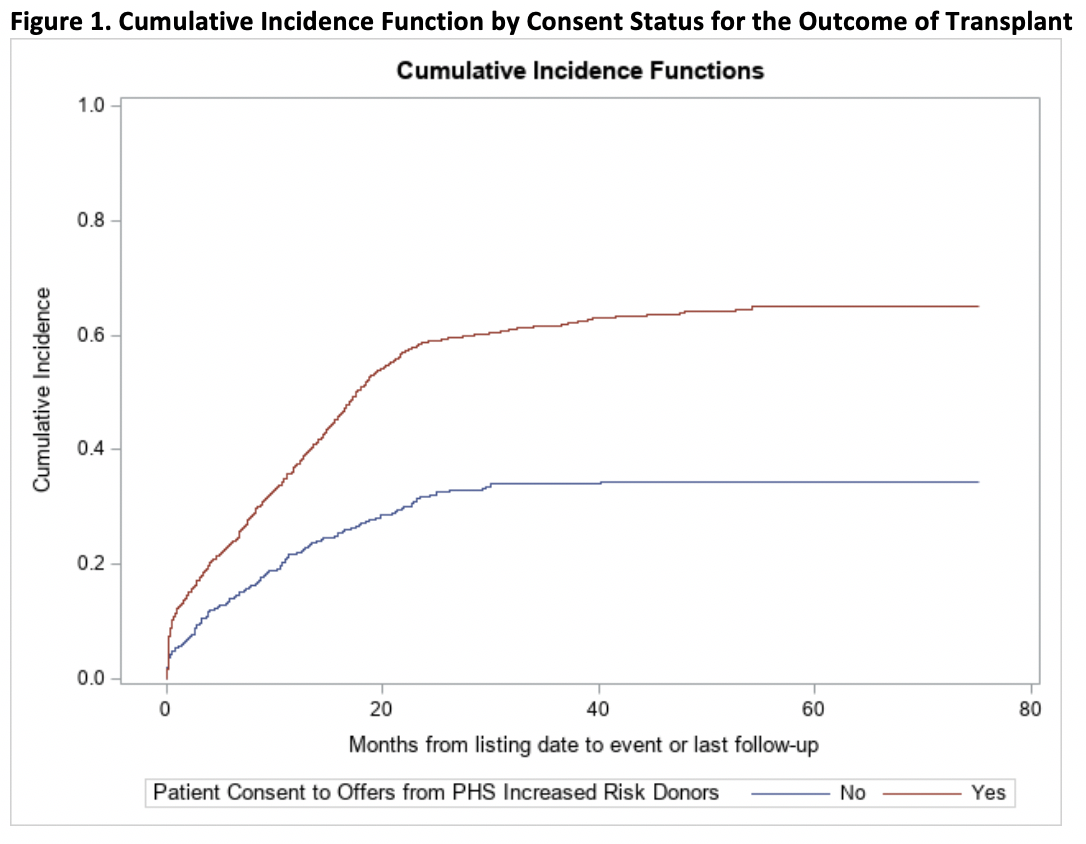
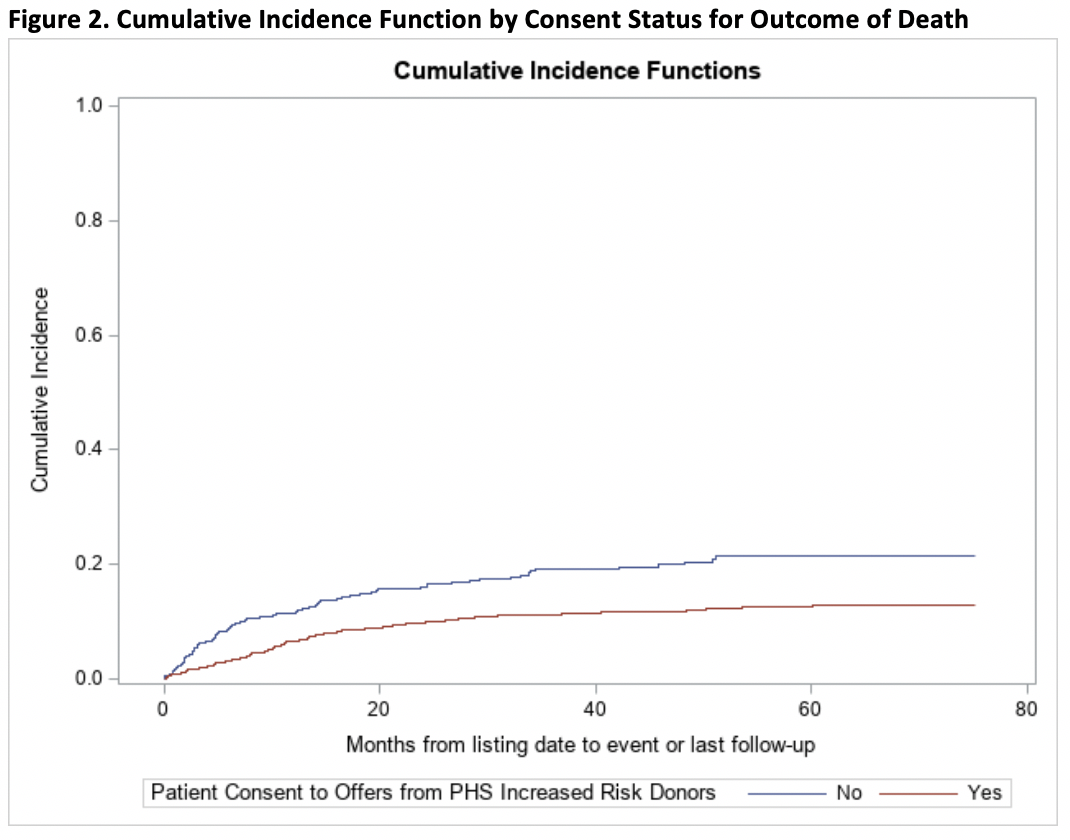
Materials and Methods: We performed a single-center retrospective review of all-comers waitlisted for liver transplant from 2013 to 2019. The three competing risk events (transplant, death, and removal from transplant list) were summarized using cumulative incidence functions (CIFs) by consent status. The association between consent status and the competing events was evaluated using Fine-Gray subdistribution hazard model, with consent to organ offers from PHS-IR donors as a covariate. To control for potential confounding effects, multivariate analyses were also performed by including recipient age at listing, race, gender, blood type, and MELD at listing as covariates in the Fine-Gray models.
Results: A total of 1,639 patients were included in the analysis, of which 1,276 (77.9%) consented to offers from PHS-IR donors and 363 (22.1%) did not. Of those who consented to PHS-IR offers who received transplants, only 192 were from PHS-IR donors. Compared to those who did not consent to PHS-IR offers, those who did consent had 2.3 times the rate of transplant (SHR 2.29, 95% CI 1.88-2.79, p<0.0001), with a median time to transplant of 11 versus 14 months. They also had a 45% decrease in the rate of death (SHR 0.55, 95% CI 0.41-0.73, p<0.0001). After controlling for recipient age at listing, race, gender, blood type, and MELD at listing, those who consented to offers from PHS-IR donors had 2.2 times the rate of transplant (SHR 2.22, 95% CI 1.79-2.75, p<0.0001) and a 51% decrease in the rate of death (SHR 0.49, 95% CI 0.36-0.65, p<0.0001).
Conclusion: Patients who consented to receiving organ donation offers from PHS-IR donors had a significantly increased rate of transplant and decreased mortality rate, even after controlling for recipient age at listing, race, gender, blood type, and MELD at listing. These findings, together with the data on low rates of disease transmission, further strengthen the case for the benefits of consenting to offers from PHS-IR designated donors.