Should steatotic livers be transplanted into pediatric recipients?
Malcolm MacConmara1, Cyrus Feizpour1, Amal Aqul2, Dev Desai1, Steven Hanish1, Lucia De Gregorio1, Parsia Vagefi1, Christine Hwang1.
1Surgery, UT Southwestern Medical Center, Dallas, TX, United States; 2Pediatrics, UT Southwestern Medical Center, Dallas, TX, United States
Introduction: Although steatotic livers are frequently transplanted in adult recipients, they are not commonly utilized in pediatric transplantation. We questioned if the outcomes of steatotic livers in pediatric recipients are comparable to non-steatotic livers and if increased utilization of these livers might be considered.
Methods: The UNOS database was used to examine outcomes in all pediatric liver transplant recipients (>18 years) who were transplanted between 2006 —2018. Recipients of living donor and multi-organ transplants were excluded. Livers were considered to be steatotic if a biopsy showed >5% macrosteatosis. Donor and recipient demographic data were examined, as were survival and outcomes data. A p-value of <0.05 was considered to be significant.
Results: There were 7,311 pediatric liver transplants performed during the study period. 58 recipients received a steatotic liver while 7,253 were transplanted with a non-steatotic liver. Recipients of the steatotic livers were more likely to be older (8.8 vs. 5.0 years), have a higher final MELD/PELD score (21 vs. 14), and less likely to have had previous abdominal surgeries. There were no differences in BMI or length of stay. Donors with steatosis were older (27.1 vs. 11.3 years) and had a greater BMI (25.2 vs. 19.7 kg/m2). Percentage of macrosteasosis in the steatotic livers was 17.5% vs. 1.4% in the non-steatotic livers. There were no differences in cold ischemia time, distance to transplant center, or transaminases. Allograft survival was also not significantly di!erent between the two groups (Figure 1). Primary non-function, acute and chronic rejection, vascular thrombosis, and biliary complications were also similar between groups.
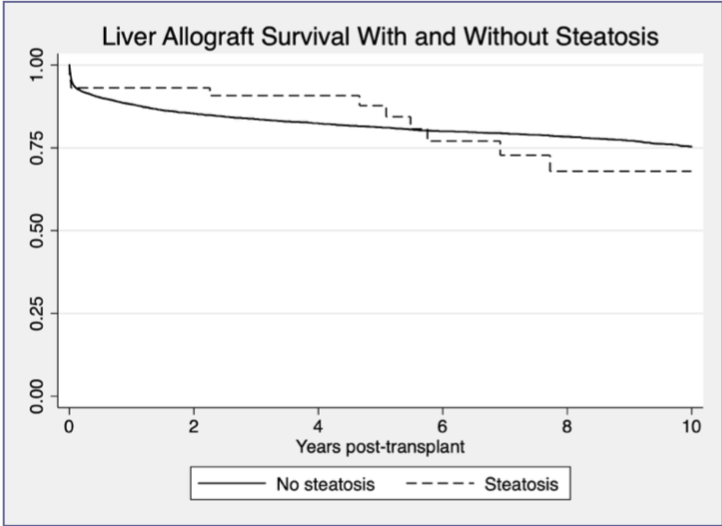
Conclusions: Pediatric patients who receive biopsy proven steatotic livers have similar outcomes to those with non-steatotic livers. With appropriate donor and recipient selection the utilization of steatotic livers can be used to expand the pediatric donor pool with good short and long-term outcomes.
