Clinical significance of pretransplant donor-specific HLA antibodies in kidney transplant recipients of hispanic population
Idalia Parra-Avila1, Abraham Cohen-Bucay1, Rogelio E. Castillo-Ramirez1, Silvia E. Ramirez-Andrade1, Luis E. Morales-Buenrostro1.
1Department of Nephrology and Transplant, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Mexico City, , Mexico
Introduction: Donor-specific HLA antibodies (DSA) before kidney transplantation (KT) is one of the major risk factors for humoral rejection and lower graft survival (1-2). In order to identify prognostic factors and develop follow up strategies in this high risk population, it is required for transplant center to share their outcome data (3-4). In addition, in most previous studies the Hispanic population is poorly represented.
Materials and Methods: Retrospective cohort and comparative study in KT recipients with pretransplant DSA measured by Luminex, negative AHG-CDC-XM (living and deceased donor) and negative flow cross match (living donor). Our main objective was to determine graft survival and describe the incidence of acute rejection (AR) and renal function (eGFR by CKD-EPI).
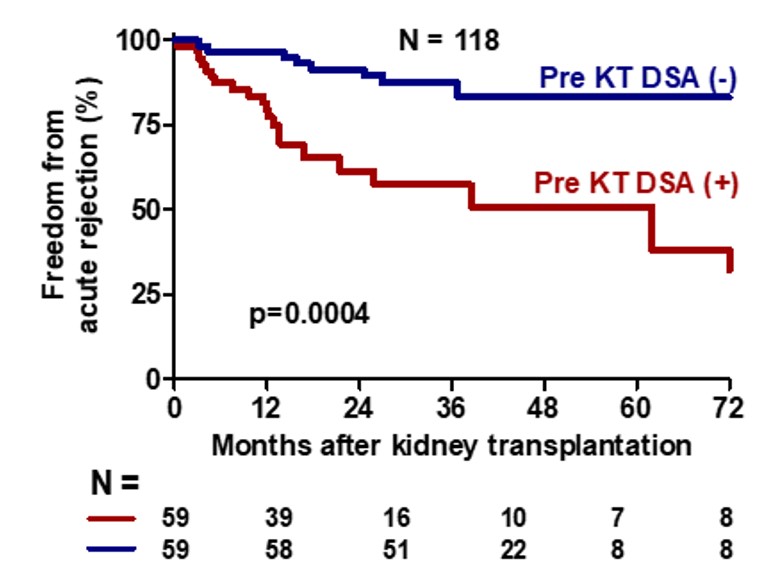
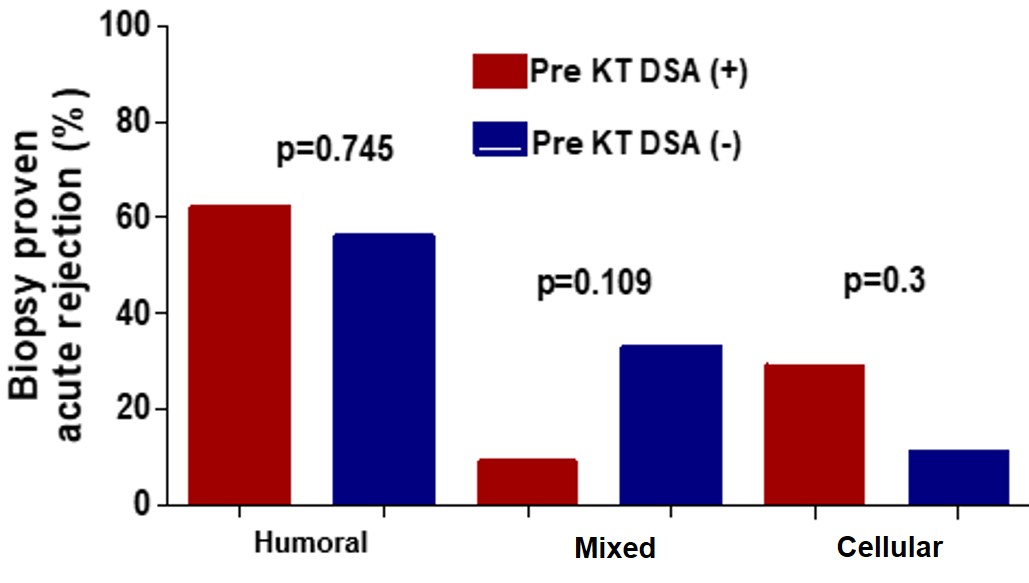
Results: Between September 2006 and March 2017, 411 patients received KT in the INCMNSZ, 60 were identified with pretransplant DSA and compared with 60 KT recipients without pretransplant DSA, paired by donor type, induction and maintenance immunosuppression. Median age was 33 (range 27-44) years, 55 (45%) were women, 55 (45.8%) had unknown etiology of ESRD, months on dialysis [24 (range 12-48)], 10.7% received second KT, 63.3% were living donor receptor, 75% had thymoglobulin induction, 96% were with tacrolimus, mycofenolate mofetil and steroids as maintenance immunosupression. The incidence of AR was increased in the pretransplant DSA group (35.5% vs. 15.2%, p=0.011) and the median time between KT and AR episodes was lower in the pretransplant DSA group [12.8 (8.3-23.6) vs 32.1 (25.9-40.6), (p<0.0001)] months.
In the pretransplant DSA group 52.4% of the biopsies with AR were protocol biopsies and 29% were secondary to graft disfunction.
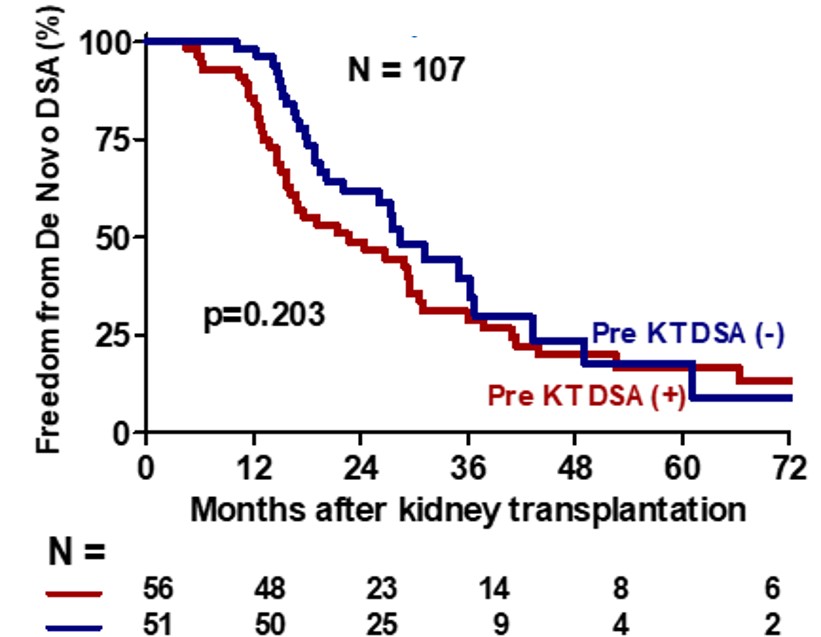
Incidence of De Novo DSA were similar between groups [30 (53.6%) vs 29 (56.8%), (p=0.732)].
After 37.4 (range 29.2-52.3) months of follow up, eGFR was similar between groups 65.0 ± 22.0 vs 69.8 ± 21.4 ml/min/1.73m2 (p=0.19) and there were no difference in graft survival (87.7% vs 96.7% p=0.240) between pretransplant DSA and without pretransplant DSA groups, respectively.
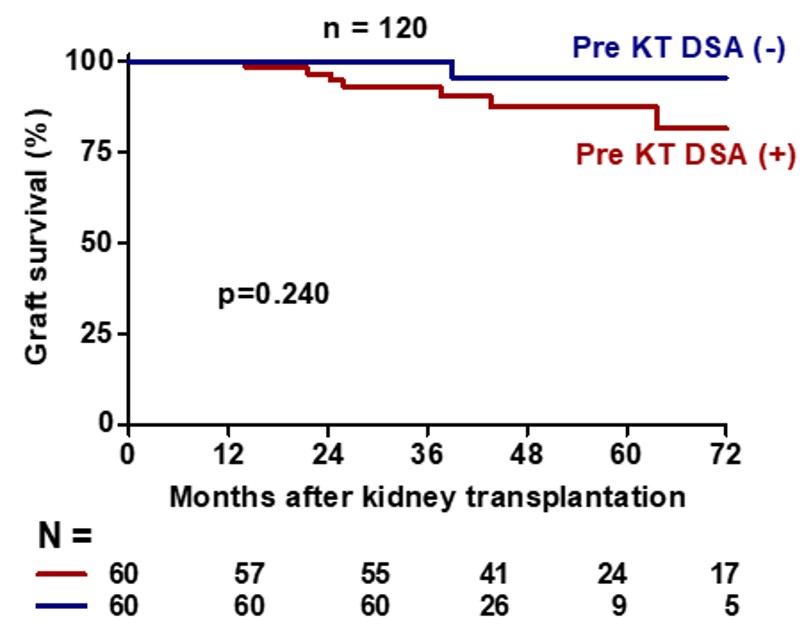
Discussion and conclusions: Although there is a higher incidence of rejection, KT recipients with pretransplant DSA could be considered candidates for KT. One limitation of this study is the small sample size and short follow-up time. However, we acknowledge that in this population of high immunological risk, induction therapy with lymphocyte depletors and powerful maintenance immunosuppression, combined with follow-up strategies as protocol biopsies with early treatment of subclinical rejection could provide similar graft survival compared to KT receptors without pretransplant DSA.
[1] Sumit Mohan , Amudha Palanisamy, Demetra Tsapepas, et al. Donor-specific Antibodies Adversely Affect Kidney Allograft Outcomes. J Am Soc Nephrol. 2012 Dec;23(12):2061-71. doi: 10.1681/ASN.2012070664.
[2] E G Kamburova , B W Wisse , I Joosten, et al. Differential Effects of Donor-Specific HLA Antibodies in Living Versus Deceased Donor Transplant. Am J Transplant. 2018 Sep;18(9):2274-2284. doi: 10.1111/ajt.14709
[3] Xicohténcatl Ixtlapale-Carmona , Adriana Arvizu , Adrian De-Santiago, et al.Graft Immunologic Events in Deceased Donor Kidney Transplant Recipients With Preformed HLA-donor Specific Antibodies. Transpl Immunol. 2018 Feb;46:8-13. doi: 10.1016/j.trim.2017.09.006
[4] Araminta Guichard-Romero , Lluvia Aurora Marino-Vazquez , Natalia Castelán , et al. Impact of Pretransplant Exposure to Allosensitization Factors Generating HLA Antibodies in the Luminex Era Transpl Immunol. 2016 Sep; 38, 33-9 DOI: 10.1016/j.trim.2016.08.003

LORENA NORIEGA-SALAS
2020-09-17 14:55
Congratulations.