Perceived vs. verified risk of cancer transmission from deceased organ donors: a 2010-2015 cohort study using data linkage in New South Wales, Australia
James A. Hedley1,2, Nicole De La Mata1,2, Brenda M. Rosales1,2, Karen M.J. Waller1,2, Imogen K. Thomson1,2, Patrick J. Kelly1,2, Michael J. O'Leary3, Elena Cavazzoni3, Kate R. Wyburn1,4,5, Angela C. Webster1,2,6.
1Centre for Organ Donation Evidence, Faculty of Health and Medicine, University of Sydney, Sydney, Australia; 2Sydney School of Public Health, Faculty of Health and Medicine, University of Sydney, Sydney, Australia; 3New South Wales Organ and Tissue Donation Service, Sydney, Australia; 4Sydney Medical School, Faculty of Health and Medicine, University of Sydney, Sydney, Australia; 5Renal Department, Royal Prince Alfred Hospital, Sydney, Australia; 6Centre for Transplant and Renal Research, Westmead Hospital, Sydney, Australia
Introduction: Donor suitability assessment is often time-sensitive, with imperfect information available at referral. Opportunities for donation may be missed if donors are rejected based on inaccurate information.
Aims: We sought to compare assessment of cancer transmission risk based on information available at referral (perceived) versus subsequently obtained (verified) detailed medical history, and to identify any missed opportunities for donation.
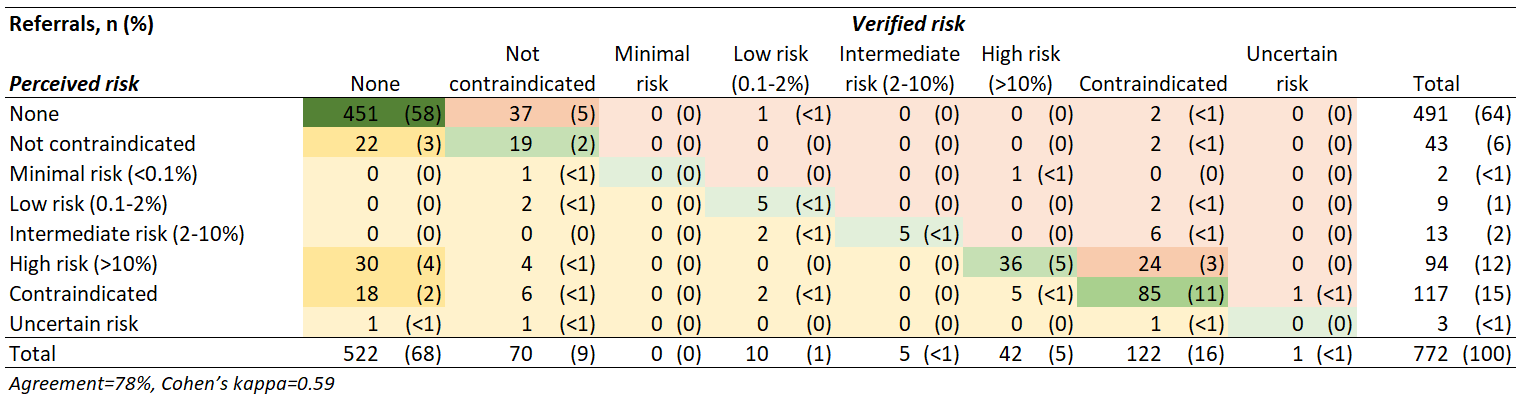
Methods: Cohort study of deceased organ donor referrals in New South Wales (NSW) 2010-2015 from the NSW Biovigilance Register. Referrals from NSW who had consent and were otherwise suitable for donation (except for perceived or verified tumour) were analysed. Perceived tumour details were obtained from NSW Organ and Tissue Donation Service referral logs, while verified details were based on the Central Cancer Registry and Admitted Patient Data Collection. Cancer transmission risk was graded using Transplantation Society of Australia and New Zealand guidelines.
Results: Among 772 referrals otherwise suitable for donation, 601 (78%) had accurately classified cancer transmission risk (κ=0.59). Overall, 53 suitable referrals were rejected due to cancer transmission risk (missed opportunities), including 49 (92%) with overestimated risk (perceived high, verified low/none), and 4 (8%) due to excessive risk aversion (perceived and verified low risk). Missed opportunities had overestimated transmission risk for tumours including leukaemia (8, 16%), lung (8, 16%), melanoma (7, 14%), brain (6, 12%), and breast (6, 12%).
Conclusions: Despite time pressure and limited information availability, there is moderate agreement between perceived and verified cancer transmission risk. Nevertheless, improved information availability (e.g. via data linkage) could meaningfully increase the number of actual donors.
There are no comments yet...
