Health professional level barriers to living donor kidney transplantation: A mixed methods study
Renata Iskander1, Marcelo Cantarovich1, Nandini Dendukuri1, Marie-Chantal Fortin2, Ahsan Alam1, Julio F. Fiore Jr1, Catherine Weber1, Shaifali Sandal1.
1McGill University, Montreal, QC, Canada; 2University of Montreal, Montreal, QC, Canada
Purpose: Despite the benefits of living donor kidney transplantation (LDKT), rates are declining across multiple centres. Efforts to increase LDKT have focused on patient-level barriers. Health professionals (HPs) play an important role in the decision to pursue LDKT, but barriers HPs identify and experience are rarely addressed. The objective of this study was to identify, quantify, and compare HP-level barriers to LDKT across three provinces in Canada with low, moderate, and high LDKT rates. We hypothesized that HP-level barriers directly correlate with LDKT rates.
Methods: We first conducted a preliminary qualitative study to explore barriers HPs experience when discussing LDKT with patients. Using this data, we identified predominant themes, which were used to create a 24-item survey instrument. We calculated the required survey sample size to be 85 participants per province. Recruitment entailed purposive criterion sampling and snowball sampling.
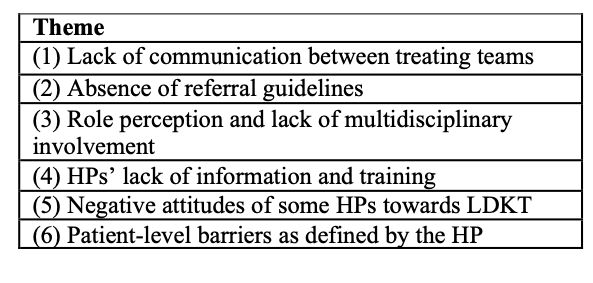
Results: In our qualitative analysis, we interviewed 16 HPs and six predominant themes of HP-level barriers to LDKT were identified.
A survey was created and pilot tested among 19 HPs, leading to preliminary results. HPs included nurses, social workers, transplant coordinators, and nephrologists from BC, ON, and QC. Among the current respondents, 89% believe that LDKT is the gold standard treatment for patients with advanced kidney disease. Only 16% perceive themselves as a part of both dialysis and transplant teams. Seventy-nine percent felt that dialysis and pre-dialysis teams should be responsible for LDKT promotion. Also, 16% felt that promoting LDKT was not part of their current role. Two-thirds felt comfortable discussing LDKT with patients and donors. More than half of respondents reported that they would discuss LDKT more with patients if they had more resources. None of the respondents believe it is ethically unacceptable to take a kidney from a healthy person; however 11% reported knowing other HPs who have a negative attitude towards LDKT. While many HPs in our qualitative study reported patient-level factors as impediments to discussions about LDKT, 88% would not change their recommendation or encourage patients to pursue LDKT over deceased donation unless a patient’s cultural background opposed LDKT. In that case, about 53% were less likely to recommend LDKT. Recruitment is still ongoing to reach the sample target to conduct a comparative assessment across provinces.
Discussion: This preliminary analysis suggests that poor role perception is a major barrier to LDKT and dedicated personnel championing LDKT are needed. Many HPs are comfortable discussing LDKT with patients and donors, but more time and resources would assist their efforts.
Conclusion: There are significant barriers to LDKT at the level of the HPs that may be directly contributing to variable rates of LDKT. Understanding these barriers and implementing strategies to alleviate them may help increase LDKT.
Canadian Institutes of Health Research (CIHR) Institute Community Support Travel Award .
There are no comments yet...
