Brain death donation improvement areas: Procurement impact
Olga Estefanía Olvera 1, María del Pilar Domínguez 3, Bertha A. García 2, Carlos Ocampo 2.
1Emergency department , Hospital General Dr. Gaudencio Gonzalez Garza Centro Médico Nacional La Raza , Mexico City , , Mexico; 2Coordinación de donación de órganos y tejidos con fines de trasplante , Hospital de Especialidades Dr. Antonio Fraga Mouret Centro Médico Nacional La Raza, Mexico City , , Mexico; 3Departamento de Investigación y educación en salud, Hospital de Especialidades Dr. Antonio Fraga Mouret Centro Médico Nacional La Raza , Mexico City , , Mexico
Introduction: in Mexico, there are 23,158 patients registered in the national organ and tissue transplant waiting list. The procurement of grafts from expanded criteria donors is justified by the increasing demand, however, not even all standard grafts have been procured. The objective was to identify the associated factors to decision making of whether to procure, or not, grafts from brain death (BD) donors in whom multiorganic donation was consented.
Methods: retrospective cohort, univariate and multivariate analysis. 35 donation files with BD were included from 2014 to 2019. Two groups were compared, the donors in which the heart wasn´t procured versus those that was procured, same comparisons were done for liver, kidney, skin, bone tissue and corneas.
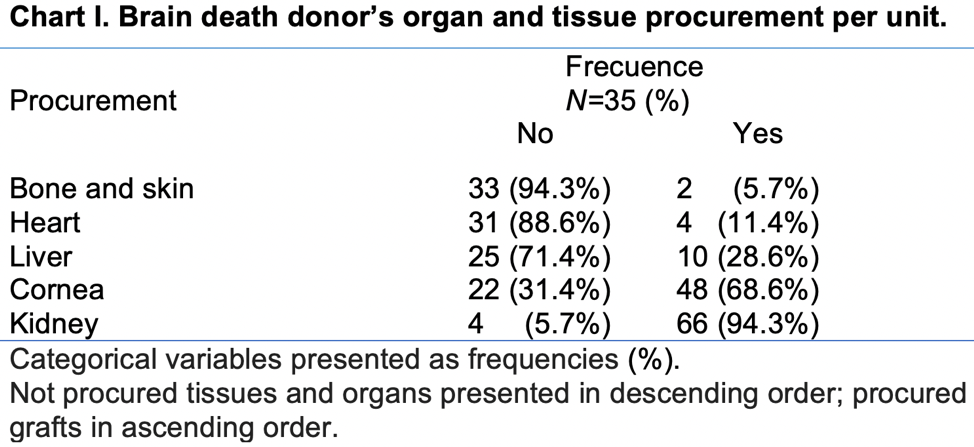
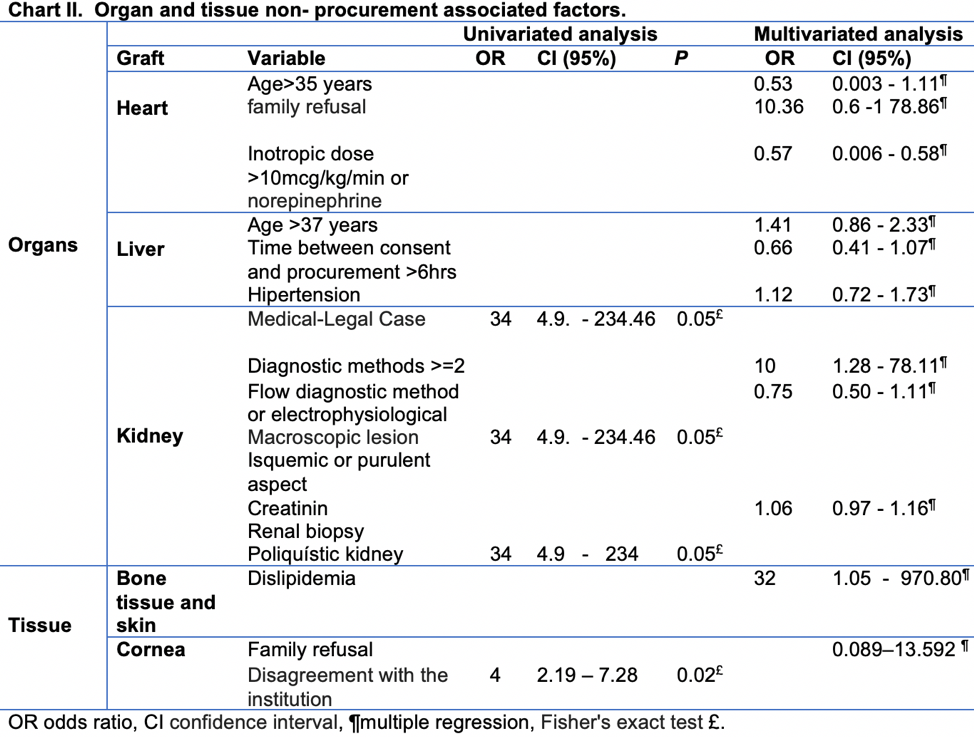
Results: 20 women (57.1%), 15 men (42.9%) average age of 43.8 ± 16.4 years. High-dose of inotropic or norepinephrine use favored cardiac procurement OR 0.57 (CI 0.0-0.5). None sensitive and specific variable was detected for decision making at liver procurement.
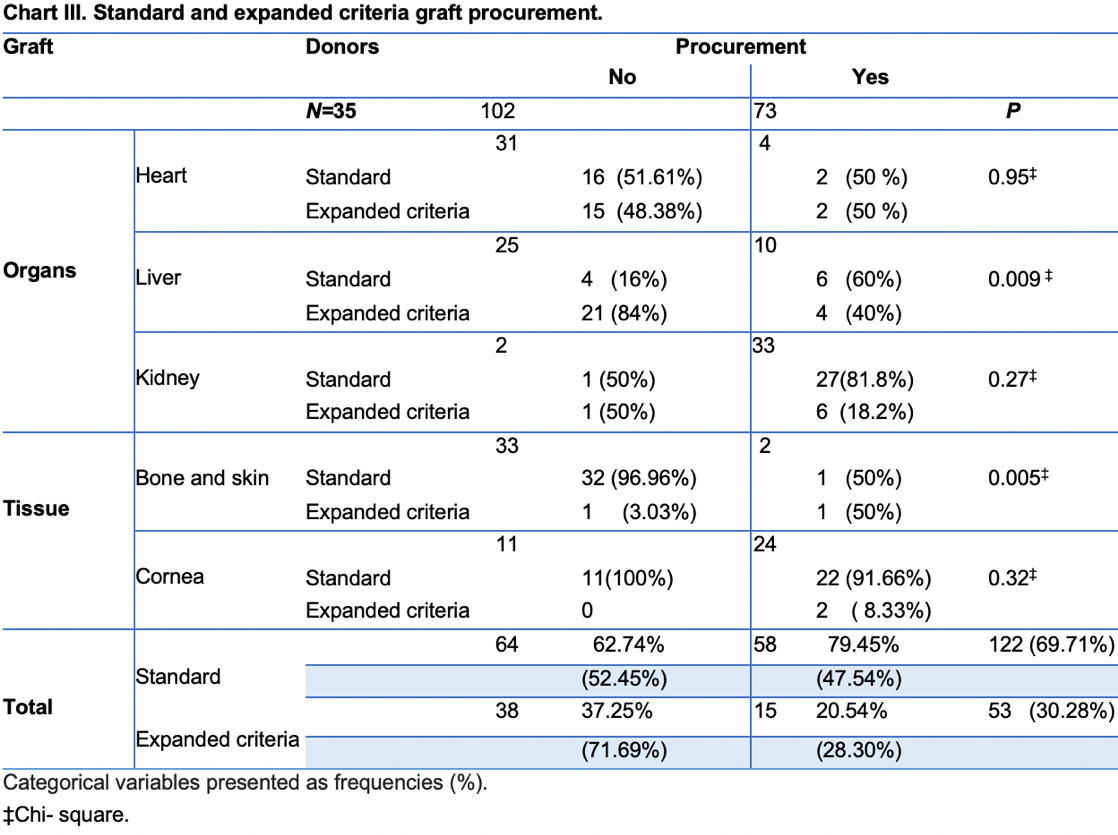
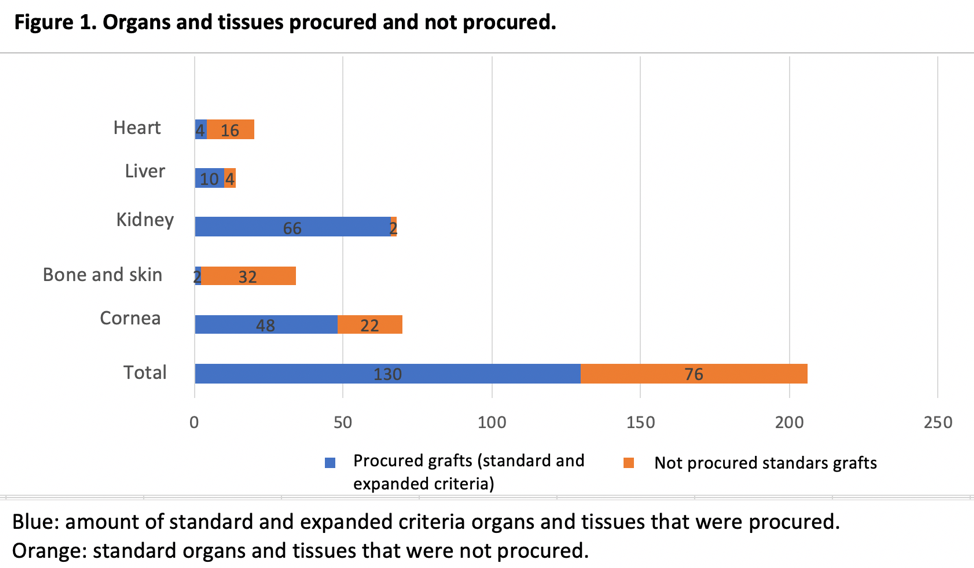
Implementation of two or more diagnostic methods for BD were associated with kidney loss OR 10 (CI 1.2-78.1). Dyslipidemia was an associated factor for non-procurement of skin and bone tissue OR 32 (CI 1.05-970.8) and family disagreement with health care institution for cornea OR 4 (CI 2.1-7.2). 183 (74.6%) organs and tissues met standard criteria, however 76 (41.5%) were not procured.
Conclusions: Non-procurement associated factors were different from the standard donor established criteria. An opportunity area is to follow clear procurement criteria in order to reduce viable grafts loss.
[1] 1. Escudero D, Otero J. Medicina intensiva y donación de órganos. ¿Explorando las últimas fronteras? Med Intensiva. 2015; 39 (6): 366-374.
[2] 2. gob.mx/cenatra [Internet]. México: Centro Nacional de Trasplantes; c2019. [Actualizado 3 Ene 2020; citado 23 Feb 2020]. Disponible en: https://www.gob.mx/cms/uploads/attachment/file/529918/4toTrimestre2019.pdf
[3] 3.Razdan M. Degenholtz H. Kahn J. Driessen J. Breakdown in the organ donation process and its effect on organ availability. Journal of Transplantation. 2015:1-7.
[4] 4.European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Liver Transplantation. Elsevier. J Hepatol 2016; 64: 433-485
[5] 5. Martínez-Vaquera S, Navarro MD, López-Andreu J, Jurado JM, Haad CR, Salas RO. Et al. Outcomes in renal transplantation with expanded- criteria donors. Elsevier. 2013; 45 (10): 3595-3598.
[6] 6. Martínez-Flores F, Sandoval-Zamora H, Machuca-Rodriguez C, Barrera-López A, García-Cavazos R, Madinaveitia-Villanueva JA. Banco de piel y tejidos: un modelo operativo para la recuperación y preservación de aloinjertos de piel y tejidos. Cirugía y Cirujanos. 2015; 84(1): 85-92.
[7] 7. Seguchi O, Fujita T, Murata Y, Sunami H, Sato T, Wantabe T. Et al. Incidence, etiology, and outcome of primary graft dysfunction in adult heart transplant recipients: a single - center experience in japan. Heart Vessels. 2016; 31 (4): 555-62.
[8] 8. Chamorro-Jambrina C, Muñoz-Ramìrez MR, Martinez-Melgar JL Pèrez-Cornejo MS. Organ donor management: Eight common recommendations and actions that deserve reflection. Med Intensiva. 2018; 41 (9): 559-568.
[9] 9. Vodkin I, Kuo A. Extended criteria donors in liver transplantation. Clin Liver Dis. 2017; 21 (2): 289-301.
[10] 10.Ko KJ. Kim YH. Kwon KH. Kim MH. Jun KW. Hwang JK. Et al. Kidney transplantation using expanded criteria deceased donors and non-expanded-criteria deceased donors. Transplant Proc. 2018; 50 (10): 3222- 3227.
[11] 11. Escudero D, Matesanz R, Soratti CA, Flores J. Muerte encefálica en iberoamérica. Med Intensiva. 2009; 33 (9): 415-423.
[12] 12. Miller C, Breakwell R. What factors influence a family’s decisions to agree to organ donation? a critical literature review. London J Prim Care. 2018; 10 (4):103-107.
[13] 13. Squires J, Graham N, Coughlin M, Chassé M, Linklater S, Greenough M. Et al. Barriers and enablers to organ donation after circulatory determination of death: a qualitative study exploring the beliefs of frontline intensive care unit professionals and organ donor coordinators. Transplant Direct. 2018; 4 (7): 1-11.
[14] 14. Matesanz R, Dominguez-Gil B. Strategies to optimize deceased organ donation. Transp Rev. 2007; 21 (4): 177-188.
There are no comments yet...
