Medium to long term impact of pre transplant DSA on allograft outcomes in deceased donors transplants
Neuza Pina1, Arun Gupta1, Cinzia Sammartino2, Ismail Mohamed2, Muhammad Magdi Yaqoob2, Raj Thuraisingham2, Delordson Kallon2, Muhammad Arslan Khurram2.
1Clinical Transplantation Laboratory, Bart’s Health NHS Trust , London , United Kingdom; 2Renal Transplantation, Bart’s Health NHS Trust , London , United Kingdom
Introduction: 26% of the patients on the waiting list in the UK are highly sensitised, which translates into difficulty in matching of suitable donors and significantly long wait times. This is associated with the risks of developing complications from long term dialysis. To counter this, one approach is transplantation despite high levels of preformed donor specific antibodies (DSAs). We compared medium to long term outcomes of deceased donor transplants between patients with preformed DSAs and non DSAs.
Methods: This is a retrospective analysis of 191 patients from a single centre between March 2008 and March 2016. All patients with ABO compatible transplants during this period with DSA or Non DSA with mean florescence intensity (MFI) of >2000 at day 0 (day of transplantation) were included in the study.
Results: There were 191 patients divided into DSA- 76 (40%) and N-DSA- 115 (60%) groups. There were more retransplants (46% v 20%), ATG usage (53% v 33%) and cRF of >80% patients (30% v 12%) in DSA group with longer cold ischaemic times (16.6 hours v 15h).
DSA group had significantly more acute (29%v10%) and chronic (13%v5%) antibody mediated rejection episodes (ABMR) compared to N-DSA. Overall, 1 year eGFR (46.7%v49.1%); 1,3 and 5 year graft survival (92%, 84%, 79% v 96%,91%, 87%) and 5 year patient survival (96%v93%) rates were not statistically different between DSA and N-DSA groups respectively (p 0.43).
In DSA subgroup, if the MFI was >8000, patients experienced more ABMR (p 0.01). 5 year graft survival was inferior with >8000MFI (48% v 99% p0.03) or positive flow crossmatch (80%v85% p0.01).
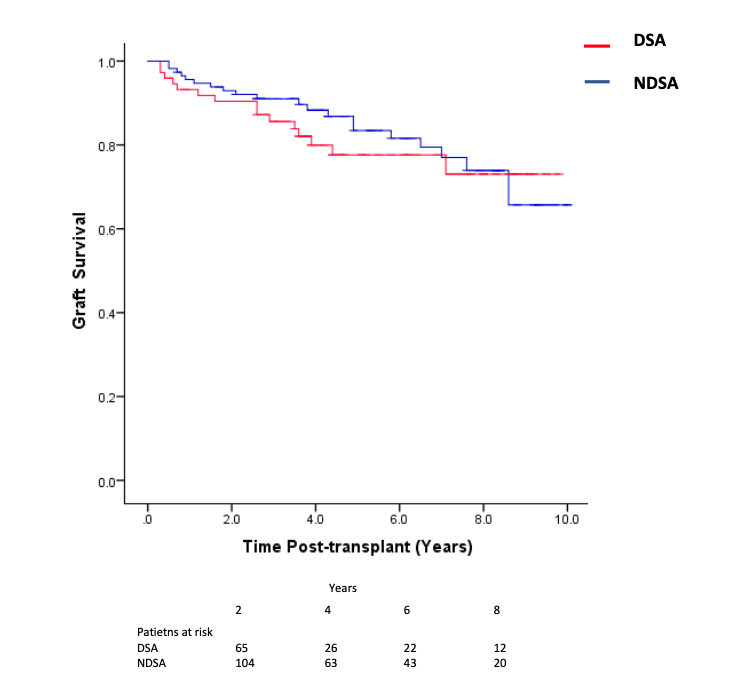
Conclusion: Overall, long term outcomes are comparable between the two groups. Careful consideration and selection must be made for patients with very high preformed DSAs.
There are no comments yet...
