Impact of induction regimen, human leukocyte antigen mismatches and steroid maintenance on recipient and graft survival with different glomerulonephridities
Samy Riad1, Scott Jackson2, Gizem Tumer3, Patrick Nachman1, Ladan Zand1.
1Medicine, University of Minnesota, Minneapolis, MN, United States; 2Complex Care Analytics, M-Health-Fairview, Minneapolis, MN, United States; 3Pathology, University of Minnesota, Minneapolis, MN, United States
Objective: Glomerulonephritis (GN) is the third leading indication for kidney transplantation. It has been hypothesized that the beneficial impact of HLA matching in patients with underlying autoimmune disorder may be offset by increased risk of graft failure due to recurrence [1,2]. We sought to assess the effect of HLA-mismatches (HLA-MM) in addition to induction agent and steroid maintenance on patient and graft survival in recipients with IgA nephropathy (IgAN), systemic lupus erythematosus (SLE), small vessel vasculitis (SVV) and anti-glomerular basement membrane disease (Anti-GBM).
Material and Methods: We analyzed SRTR standard analysis files for adult, primary kidney-alone recipients with the above glomerulonephridities through Q3 2019. We included all recipients who received induction (depletional vs non-depletional) and were discharged on tacrolimus and mycophenolate with or without steroid maintenance. Our Cohort included 9,176 IgAN, 5,355 SLE, 1,189 SVV and 660 Anti-GBM recipients. Kaplan-Meier curves were generated to examine the main outcomes of interest in each of the groups separately. Multivariate Cox proportional hazard models were utilized to examine the impact of induction regimens, HLA-MM and steroid maintenance in each of the GN groups separately. Models were adjusted for recipient and donor age, gender, race, recipients’ comorbidities including diabetes and peripheral vascular disease, pretransplant dialysis status and duration, donor type and payer type. Transplant centers were included as a random effect.
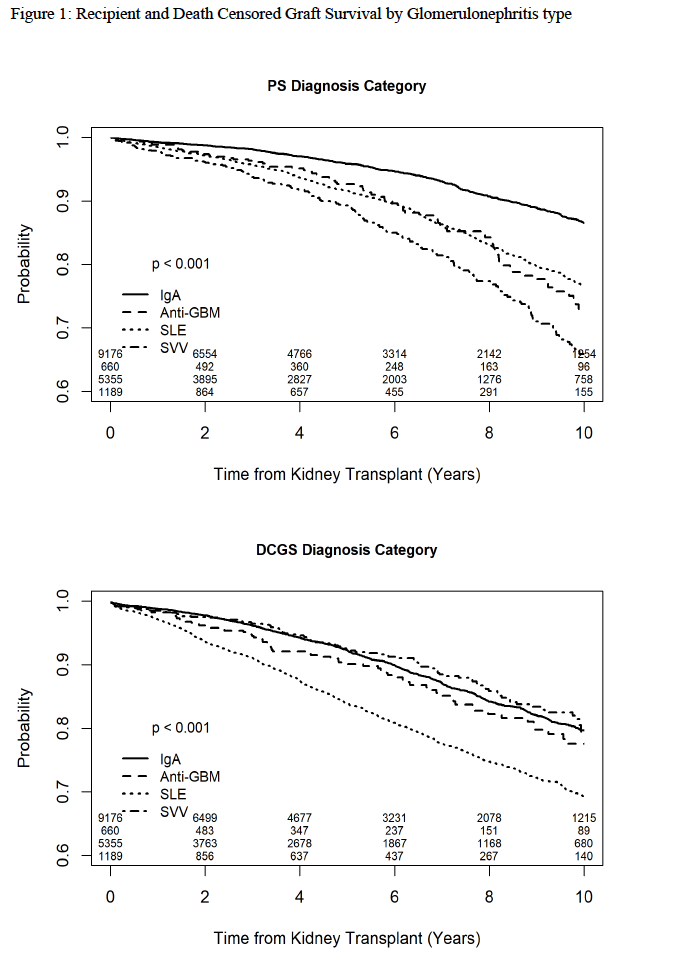
Results: Overall recipients and death censored graft survival by GN type is depicted in Figure 1.
Neither induction type nor steroid maintenance influenced recipient or death-censored graft survival (DSGS). HLA-MM were conventionally associated with decreased DSGS in patients with IgAN and SVV but had no effect on patient survival. In patients with anti-GBM and SLE, HLA matching did not improve graft survival and in patients with SLE, 6-antigen HLA matching was associated with lower patient survival. (Table 1).
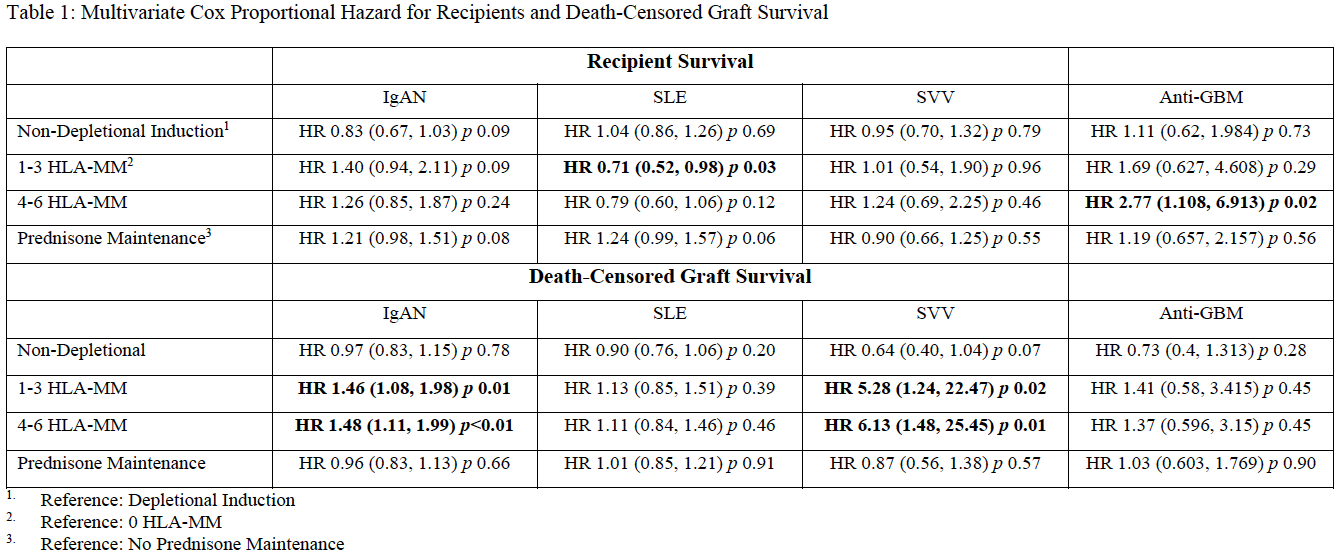
Conclusion: In this large cohort of transplant recipients with glomerulonephritis, HLA matching improved graft survival in patients with IgAN and SSV but conferred no advantage for graft survival in patients with anti-GBM and SLE. Interestingly, close HLA-Matching may pose a deleterious effect on patient survival in patients with SLE. Further studies to elucidate the underlying immunologic mechanism are needed.
M-Health Fairview. University of Minnesota.
[1] Alexander J, Lord JD, Yeh MM, Cuevas C, Bakthavatsalam R, Kowdley KV. Risk factors for recurrence of primary sclerosing cholangitis after liver transplantation. Liver Transpl. 2008;14(2):245-251.
[2] Egawa H, Ueda Y, Ichida T, et al. Risk factors for recurrence of primary sclerosing cholangitis after living donor liver transplantation in Japanese registry. Am J Transplant. 2011;11(3):518-527.
There are no comments yet...
