Lymphocytopenia and neutrophilia determined fungal infection occurrence and mortality after liver transplantation
Jiang Liu1,2, Kwan Man2, Qian Lu1, Jiahong Dong1.
1Department of Surgery, Beijing Tsinghua Changgung Hospital, Tsinghua University, Beijing, People's Republic of China; 2Department of Surgery, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong, People's Republic of China
Introduction: Fungal infection in liver recipients remains a critical challenge with high mortality and morbidity. Immunosuppression regimen renders patients more vulnerable to fungal infection after liver transplantation. However, the mechanisms of immune status and its role in predicting post-transplant mortality are still undetermined.
Materials and Methods: Adult patients received liver transplantation were recruited in a retrospective cohort from February 2018 to October 2019 in Beijing Tsinghua Changgung Hospital. The post-transplant immune cell subpopulations and peri-operation demographics were analyzed in patients with or without post-transplant fungal infections. Univariate and multivariate logistic regression were performed to identify risk factors for post-transplant fungal infections. The correlation between recipient immune status and post-transplant 90-day mortality was further investigated by ROC and Kaplan-Meier analysis.
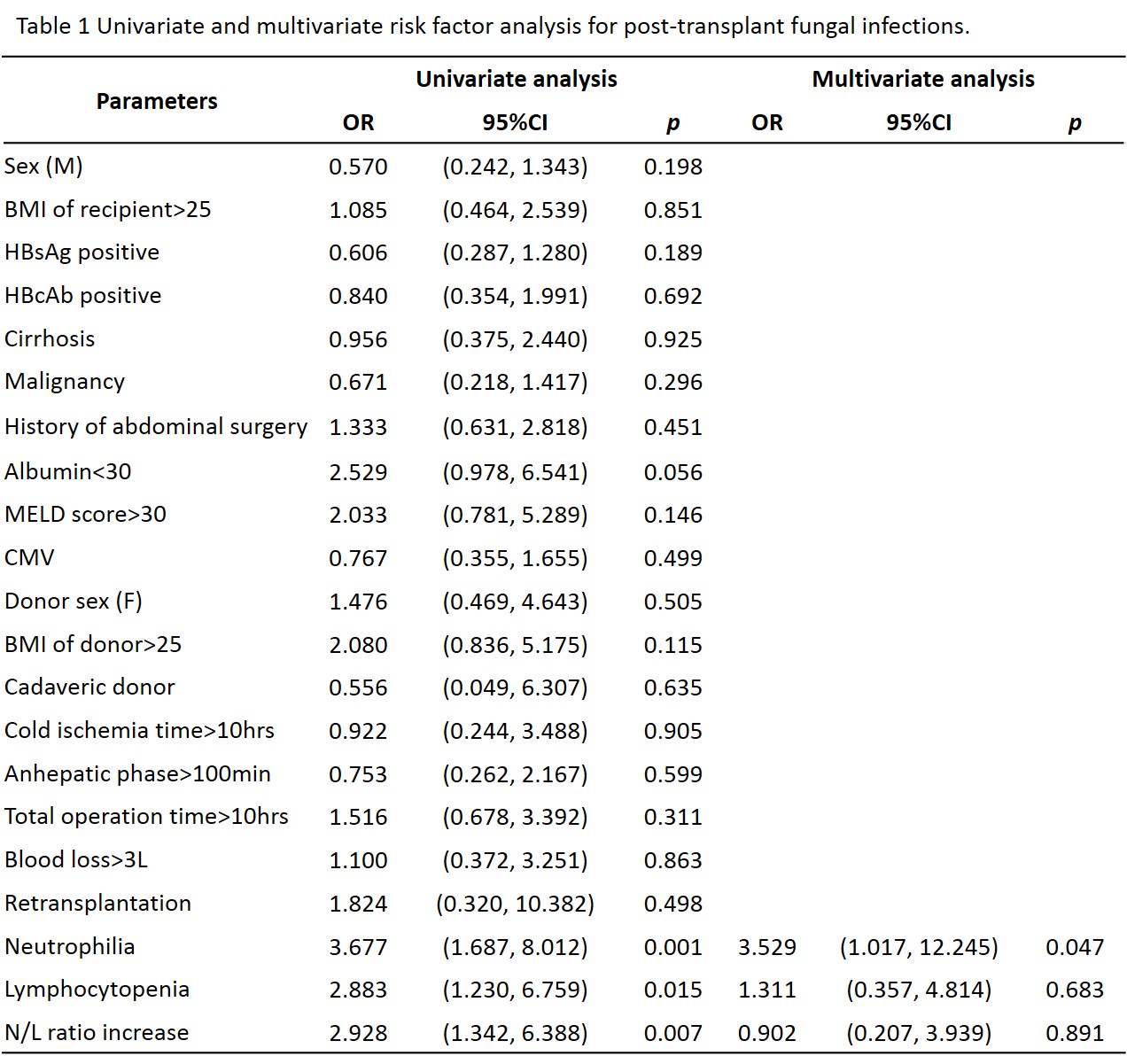
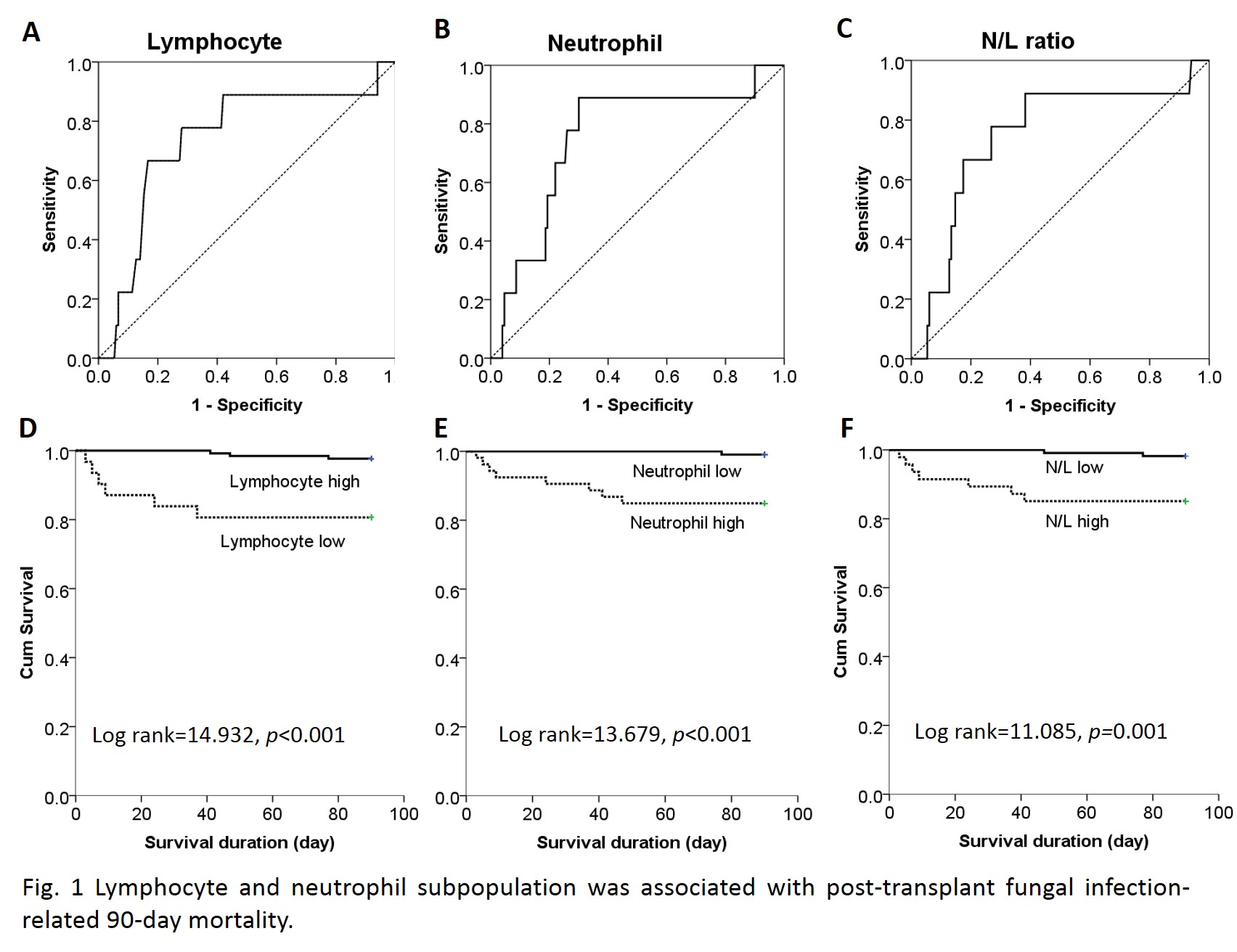
Results and Discussion: Thirty-six out of 164 (22%) patients were presented post-transplant fungal infections with median occurrence time of POD4 (1-287). In terms of fungi species, 27 (75%) were from Candida species, 6 (16.7%) were from Aspergillus species, and 3 (8.3%) were other fungal infections. And the infection site distributed in upper respiratory tract (17, 47.2%), lower respiratory tract (2, 5.6%), intra-abdominal cavity (11, 30.6%), bloodstream (3, 8.3%), urine (2, 5.6%) and wound (1, 2.8%). In comparison with non-infection patients, the lymphocyte population in blood was found significantly lower in fungal infection patients (5.0% vs 8.6%, p=0.007), while neutrophil increase was simultaneously observed (90.7% vs 83.3%, p=0.004). In addition, subpopulation analysis indicated the decrease of CD19+ B cell (26.2% vs 16.8%, p=0.069), but increase of CD3-CD16+CD56+ NK cell (7.0% vs 10.9%, p=0.001) and CD3+CD8+ CTL (20.9% vs 28.8%, p=0.120). By univariate and multivariate analysis, neutrophilia (percentage≥90.05%) was identified as an independent risk factor for post-transplant fungal infection (HR=3.529, 95%CI: 1.017-12.245, p=0.047, Table 1). By ROC analyses, lymphocytopenia and neutrophilia as well as the neutrophil-to-lymphocyte (N/L) ratio increase was found to have predictive value for 90-day mortality (Fig. 1A-C). And 90-day mortality divided by cut-off values of lymphocyte, neutrophil and N/L ratio was significantly different between groups (Fig. 1D-F).
Conclusion: Altered immune status was the independent risk factor for fungal infections after liver transplantation. Lymphocytopenia and neutrophilia, as well as increased N/L ratio, were valuable predictors of fungal infection-related post-transplant mortality.
There are no comments yet...
