More than 10 years of survival after intestinal transplant at a single center in Latin America, and its correlation with NOD2 mutations
Mariana Doeyo1, Mariana Ortega1, Gentilini Virginia2, Rumbo Carolina1, Adriana Fernandez1, Maria Ines Martinez1, Jacques Pirenne4, Laurens Ceulemans 4, Martin Rumbo3, Diego Ramish1, Hector Solar1, Gabriel Gondolesi1.
1Hospital Universitario Fundacion Favaloro, Buenos Aires, Argentina; 2Translational Research Laboratory and Immunology associated to Transplantation, Hospital Universitario Fundacion Favaloro- CONICET, Buenos Aires, Argentina; 3Immunology and Pathophysiology Studies Institute (IPSI-CONICET) School of Exact Sciences, UNLP, La Plata, Argentina; 4Department of Abdominal Transplantation Surgery, University Hospitals Leuven, Leuven, Belgium
Introduction: Intestinal transplant (ITx) remains the last therapeutic alternative for patients with intestinal failure and parenteral nutrition related complications. Although graft and patient survival have improved significantly over the last decades, very few reports of long time outcomes after ITx are available We aim to describe the outcome of all patients that survived more than 10 years after ITx at single center in Latin-America (LA) .
Materials and Methods: A retrospective analysis of a prospectively filled ITx database was done. Diagnosis, ITx indications, NOD2 mutation, incidence of rejection, and social reinsertion in patients that survived more than 10 after ITx are reported.
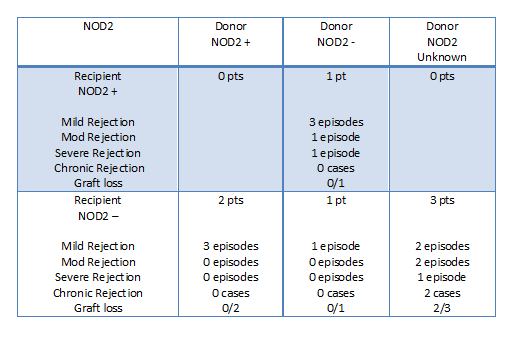
Results: A total of 50 ITx (adults and pediatric) were performed in this Unit since in May 2006. Twenty-five of them were done between 2006 and 2010, and 9 recipients (36%) are currently alive; 7 with functional grafts. Seven were pediatric patients (78%) at the time of the ITx, 6 were male (66%). All patients had short bowel syndrome, (volvulus (44%), Hirschsprung’s disease (22%), ischemia (11%), abdominal sepsis (11%) and necrotizing enterocolitis (11%). The indications for ITx were lack of central venous accesses (44%), recurrent line sepsis (33%) and IFALD (22%). Eight patients received isolated ITx and 1 a combined liver-intestine graft. Mean hospital stay after ITx was 36.75 +/- 14.97 days. In this cohort, 7 pts were evaluated for NOD2 polymorphism (m) (4 Donor (D) and Recipient (R) pairs were tested and in cases 3 only the R was tested); Only 1R was positive for NOD2 polymorphisms (14%); while 2 of the 4 D evaluated had NOD2 mutations (50%). The presence of this mutation on D and/or R and its correlation with rejections results is shown in table 1. Three patients lost the intestinal graft, (1 due to chronic rejection and 2 due to late severe exfoliative rejection [1 D NOD2+; 1 Not Available]). One patient is not eligible for re-transplantation and remains on palliative care. The other 2 R were re-transplanted;. One pt had a partial enterectomy due to chronic rejection [R NOD 2 -] but remains PN free. Complications related to long term immunosuppression include: diabetes (1), chronic renal failure requiring kidney transplant (2), bilateral aseptic necrosis of the femoral head (2) and visceral Kaposi sarcoma (1). All pts were able to resume their normal life, and 7 are currently PN free.
Conclusions: ITx has become a feasible option for IF patients who evolve with PN complications in LA, achieving long time survival under the care of a multidisciplinary team. Although retrospectively obtained, NOD2 polymorphism is, and might be consider as tool to be used in the future for organ allocation aiming to improve long-term patients and graft results, as well as for recipient follow-up; larger population studies are needed in order to validate this findings.
There are no comments yet...
