Comparison of two novel formulas to predict parenteral nutrition discontinuation in adults with Type III intestinal failure
Florencia Fernandez1, Hector Solar1, Mariana Doeyo1, Mariana Ortega1, Diego Ramish1, Adriana Crivelli1, Gabriel Gondolesi1.
1Hospital Universitario Fundacion Favaloro, Buenos Aires, Argentina
Introduction: Short bowel syndrome remains the main cause of intestinal failure worldwide. A great progress has been made over the last decade on the rehabilitation field with the introduction of autologous GI reconstruction surgeries (AGIRS) and teduglutide (TED). The challenge that still remains unsolved, is the possibility of predicting which patient will be able to recover intestinal sufficiency (IS) under the current multidisciplinary therapeutic approach, instead of predicting IS based only on anatomical variables. Two formulas have described with this purpose during the last year; one includes de impact of PN as part of a mathematical model, while the other includes TED as part of its variables.
Aim: We aim to compare those two formulas to describe its differences and to establish if they could be applied to a different group of patients.
Materials and Methods: A retrospective analysis of a prospective database of type III intestinal failure (IF-III) patients that underwent AGIRS from 03/2006 to 02/2020 was done applying both formulas to each patient with the complete set of data. (Formula A: 1/(1+(EXP(-1*(5,178-(3,866*PSIL)-(1,886*ICV)-(2,737*TED))))); Formula B: https://projects.majestictech.co.in/rna/). Positive and negative predictive value for each one was calculated by performing a ROC curve on SPSS v20.0.
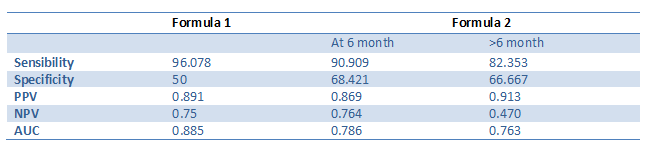
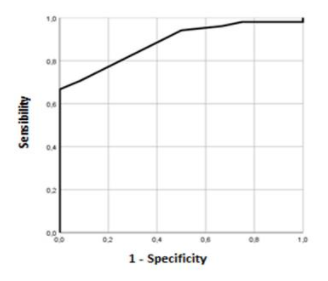
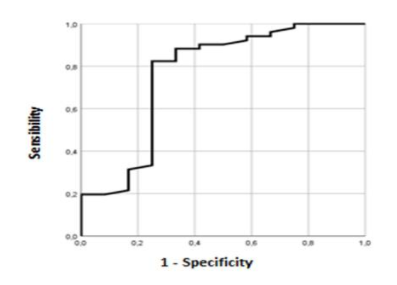
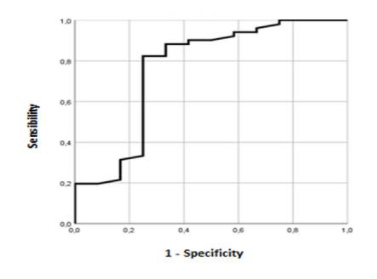
Results: From a total of 323 III-IF patients, 93 (28%) underwent AGIRS, and in 63 patients (67%) the complete information was available to perform both mathematical models. For formula A the positive predictive value (PPV) was 0.89 and the negative predictive value (NPV) was 0.75 ; with a sensibility of 96.08% and a specificity of 50%. In Formula B the PPV was 0.89, the NPV was 0.76, having a sensibility of 90.1% and a specificity of 68.4%, at 6 months after surgery (table1). When data was analyzed beyond 6 months, PPV for Formula B was 0.91, NPV was 0.47 and its sensibility and specificity were 82.38 and 66.67 respectively. Figure 1 shows the ROC analysis of both formulas.
Conclusions: This is the first study to validate and compare the described formulas, using a single set of patients; both formulas serve to determine the probability of weaning off PN in adults patients; Formula A has the highest ROC value, implying a higher sensibility, it includes as a variable the current medical therapy used for IF-III pts (TED), and it doesn’t establish a time limit to its applicability. Both formulas can be utilized before or after AGIRS. Prospective, multicenter trials on a larger population are needed to validate these results.
There are no comments yet...
