
Incidence, risk factors & patient outcomes of acute kidney injury in patients undergoing living donor liver transplant- A prospective single centre study
Abhyudaysingh Rana1, Arvinder Singh Soin2, Amit Kumar Mahapatra1, Ashwini Gadde1, Neeraj Saraf3, Shyam Bihari Bansal1.
1Nephrology and Renal Transplant Medicine, Medanta-The Medicity, Gurugram, India; 2Liver Transplant and Regenerative Medicine, Medanta-The Medicity, Gurugram, India; 3Gastroenterology & Hepatobiliary Science, Medanta-The Medicity, Gurugram, India
Introduction: AKI is common postoperative complication after liver transplant (LT). Early post transplant AKI has been associated with increased rates of acute rejection and infectious complication, longer ICU stays, higher mortality rates & poor long-term survival independent of pre transplant renal function.
There is dearth of data on AKI in patients post Living donor LT from India & abroad. Most of the studies done are on deceased donor Liver transplant, or if done on Living donor are retrospective in nature. There is inconsistency in studies regarding definition of AKI hence a prospective study to assess incidence, risk factor and patient outcomes of AKI in living donor liver transplant patients was undertaken.
Material & Method: Patients over age of 18 years undergoing living donor liver transplant at our center were selected consecutively from January 2019 to January 2020, prospectively followed for 1 month post op to assess incidence of AKI (Early-<=7, Late >7 to <30) & reassessed at 3 months for persistence of renal dysfunction. Patients with fulminant liver failure, those undergoing combined liver kidney transplant & who died within first 72 hour post-LT were excluded. AKI was defined by KDIGO criteria. Preoperative, Intraoperative & Post operative variables were analysed for risk factor & patient outcomes by regression analysis.
Results: During the study period 211 patients underwent LDLT between period of January 2019 to January 2020. After excluding patient as per exclusion criteria 185 patients were included in final analysis. Mean age of our cohort was 50.64±10.4 years & 159 (85.9%) were male.
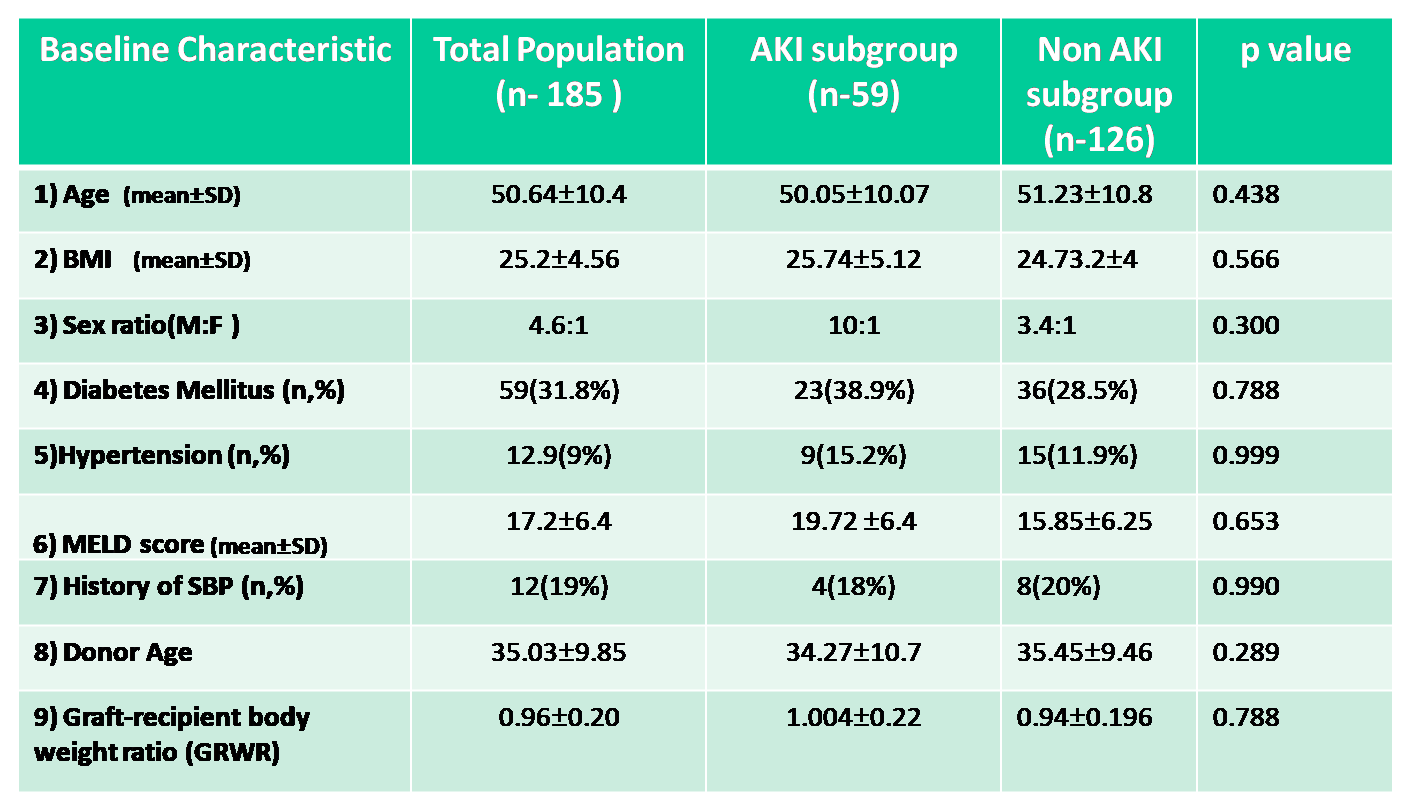
59 (31.8%) patients developed AKI. 31 (52.5%) had stage 1 AKI, 20 (33.8%) Stage 2 & 8 (13.5%) had stage 3 AKI requiring CRRT/SLED. 42 (71 %) patients had early AKI, 17 (29%) had late AKI.
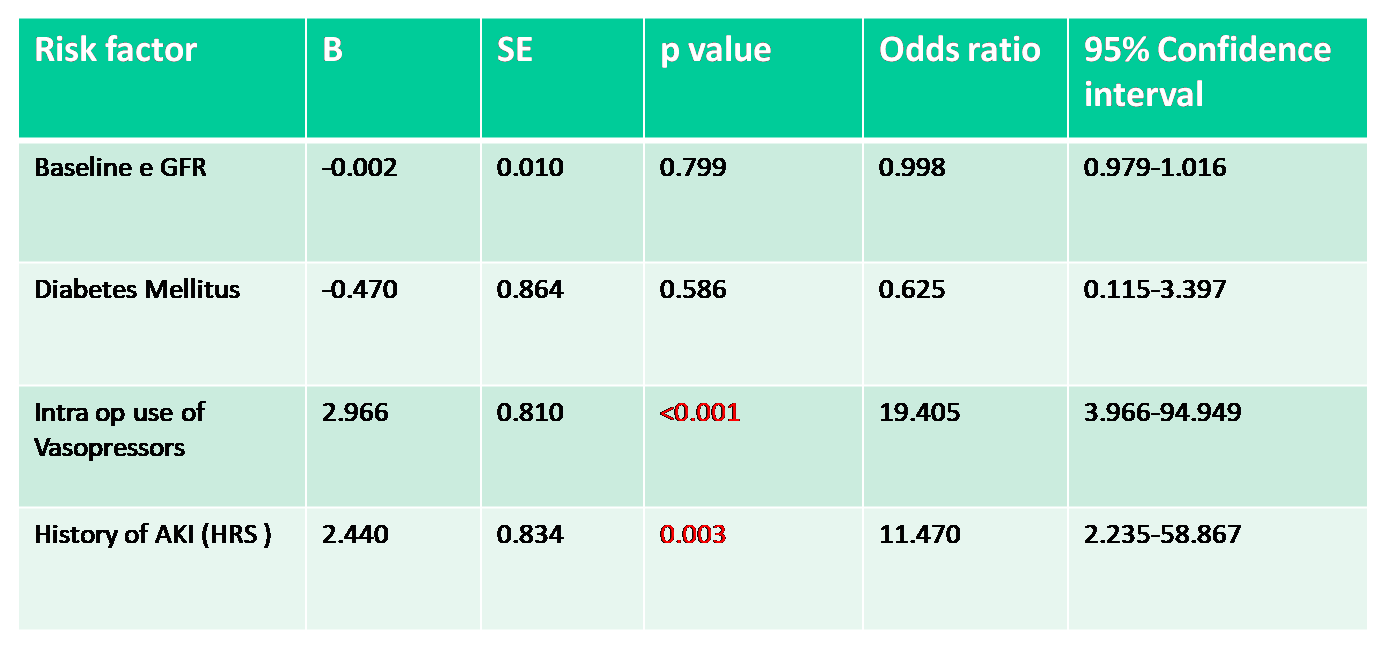
Most common cause of early AKI was multifactorial (12,28.57%). Most common cause of Late AKI was sepsis (14,82.3%). Use of vasopressors intra op & Past history of AKI (HRS) were the only statistically significant (p <0.001) risk factors for AKI.
The mean ICU stay among patients with AKI was 8±4.4 days vs 4.9±2.1 days in patients without AKI. Median days to normalization of liver enzymes in non AKI group was 10 days vs 18 days in AKI group.5 (2.7%) patient had persistence of renal dysfunction at 3 month. 26 (14.05%) patients died during analysis period, 16 (8.6%) of them from AKI group.
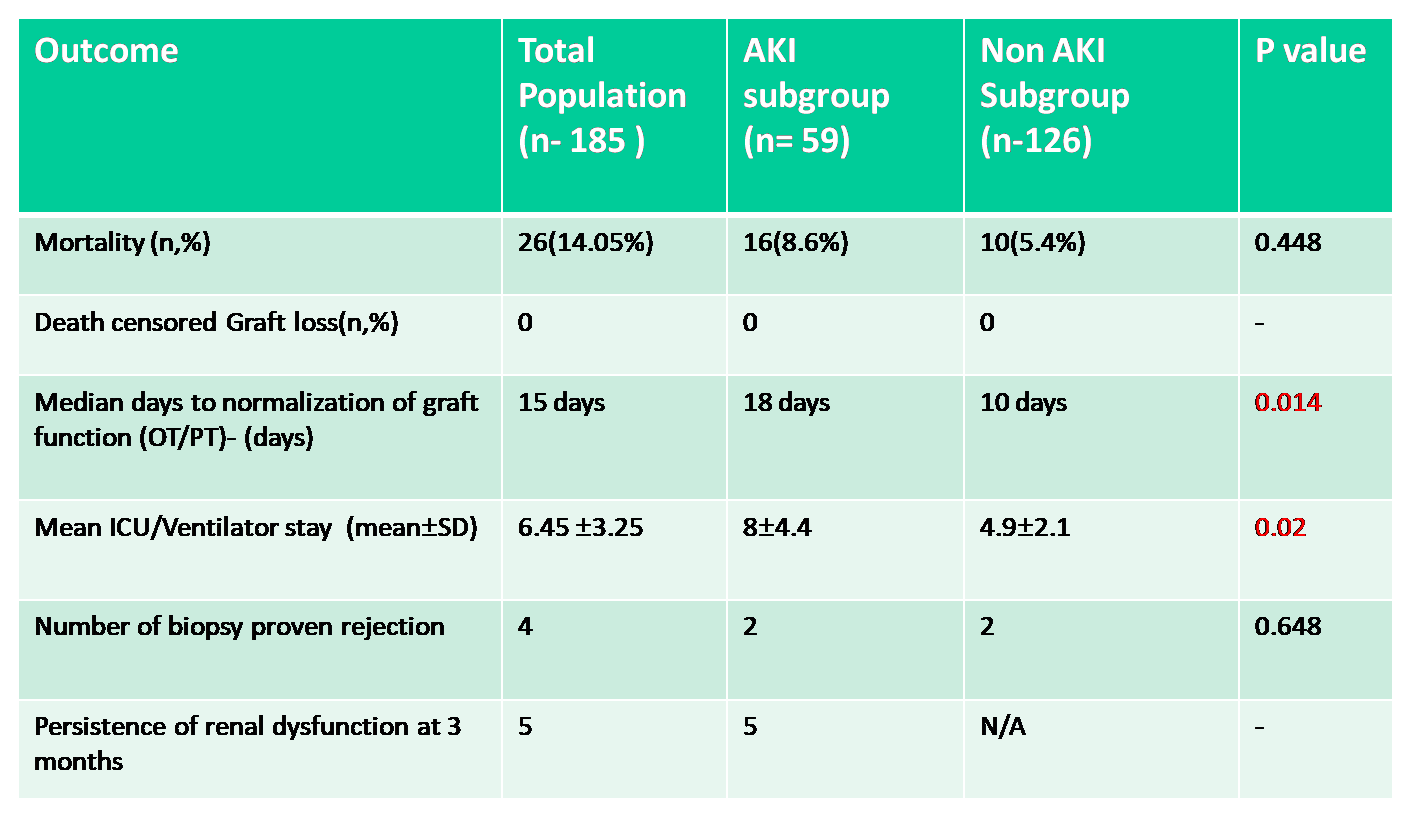
Conclusion: Incidence of AKI was 31.8 % cohort and lead to CKD in 5 patients. Use of vasopressors intra op & Past history of AKI (HRS) were risk factors for AKI in our cohort. (p<0.001). Although AKI was transient it lead to increase ICU stay and prolonged normalization of graft function in patients undergoing living donor liver transplant. AKI did not effect mortality rates.
There are no comments yet...
