Impact of donor cardiopulmonary resuscitation on long-term allograft outcome after deceased donor kidney transplantation in Thailand
Thawin Srinutta1, Korntip Phonphok1.
1Renal unit, department of internal medicine, Rajavithi Hospital, Bangkok, Thailand
Background: Despite the increasing number of deceased donors in Thailand, the availability of deceased transplant kidneys remains a challenge. In 2019, 482 deceased donor kidney transplants (KT) were performed while 6,082 candidates were waiting for a KT. Utilization of marginal donation after brain death (DBD) kidneys has risen, however, the transplant outcome has not been well studied. Therefore, we examined the impact of donor cardiopulmonary resuscitation (CPR) on the allograft outcome in Thai deceased donor KT.
Methods: We retrospectively reviewed the data of deceased donors who received KT between 1997 and 2019 from Organ Donation Centre, Thai Red Cross and the Thai Transplant Registry. We divided deceased donors according to CPR status. Data were reported as mean and standard deviation for continuous data, and frequency and percentage for categorical data. Allograft function was analyzed by using chi-square. Survival analysis was analyzed by using cox-proportional hazard model. P-value <0.05 was defined as statistically significant. Statistical analysis was performed using SPSS version 20.
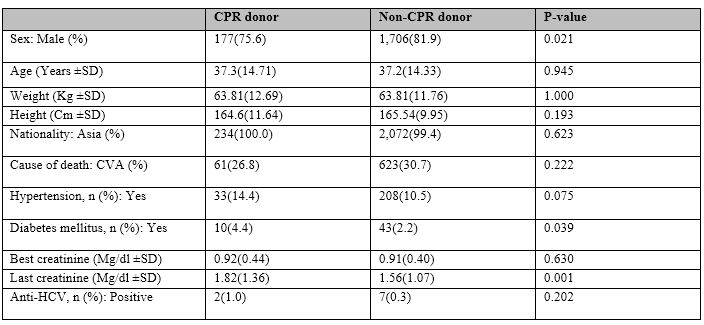
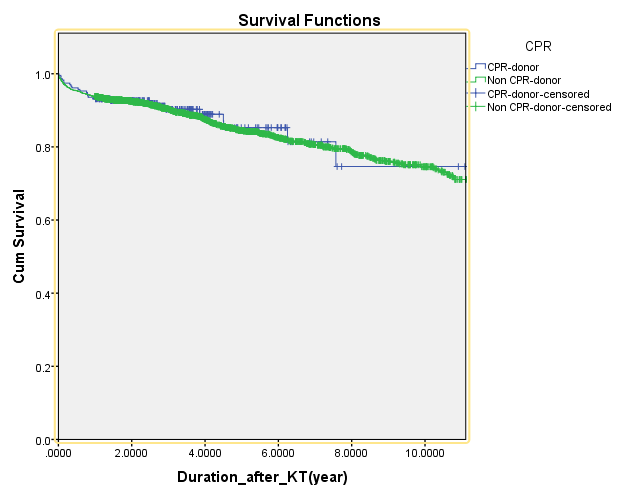
Results: The data revealed 2,318 deceased donor KT patients. Of these, 234 (10%) patients received kidneys from DBD donors with CPR. DBD donor with CPR were more likely to be female, have underlying hypertension, and diabetes, and higher terminal serum creatinine, compared to those with no CPR. (table) One-year allograft function was not different between groups (OR 1.038, 95%CI 0.597-1.804, p-value 0.895) as well as the overall graft survival. (HR 0.963, 95% CI 0.554-1.674, p-value 0.895) (figure).
Conclusion: DBD donors with CPR did not affect the long-term allograft outcome after deceased donor KT. Obtaining kidneys from a potential DBD donor with CPR with appropriate consideration of acceptance would expand the deceased donor pool with comparable allograft outcome.
Organ Donation Centre, Thai Red Cross. Thai Transplant Society.
There are no comments yet...
