Comprehensive evaluation of echocardiographic changes after kidney transplantation and long-term outcomes
Camilo Cortesi1, Madeline Chun2, Raymond Hsu1, Mai Sedki2, Mehdi Tavakol3, Brian K. Lee1.
1Division Nephrology, Department of Medicine, University of California San Francisco, San Francisco, CA, United States; 2School of Public Health , University of California Berkeley, Berkeley, CA, United States; 3Division of Transplant Surgery, Department of Surgery, University of California San Francisco, San Francisco, CA, United States
Introduction: Cardiovascular disease is one of the leading causes of death after kidney transplantation (KT). Several echocardiographic changes have been reported in advanced CKD and associated with poor outcomes after KT. Previous studies, the majority of which had small cohorts, have assessed few echocardiographic parameters after KT. We aim to provide a comprehensive evaluation of clinically relevant echocardiographic parameters pre and post-KT, and to examine their associations with allograft and patient survival.
Material and Methods: This is a retrospective cohort study of 287 adult patients who underwent ≥1 KT between 2009 and 2018 at the University of California, San Francisco Medical Center and who had complete echocardiographic assessments both pre and post-transplantation. The primary predictors were clinically relevant echocardiographic parameters abstracted from electronic health records: left ventricular ejection fraction (EF), diastolic dysfunction (DD), pulmonary artery systolic pressures (PASP), and left ventricular mass index (LVMI). Paired t-test and Wilcoxon matched-pairs signed-rank test were used to evaluate echocardiographic changes after KT. Cox proportional regression was performed to examine the associations between pre and post-KT echocardiographic parameters with death and graft loss post-KT.
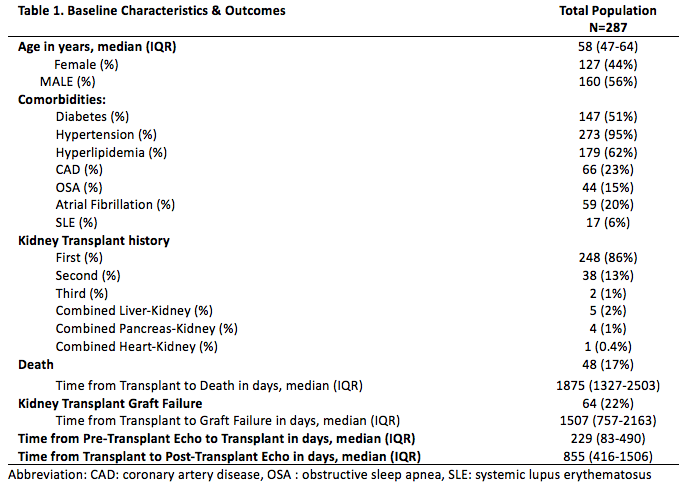
Results and Discussion: Table 1 shows the cohort's baseline characteristics and outcomes.
EF and LVMI (but not PASP) were found to have significant changes after KT (p=0.005 and p<0.0005 respectively).
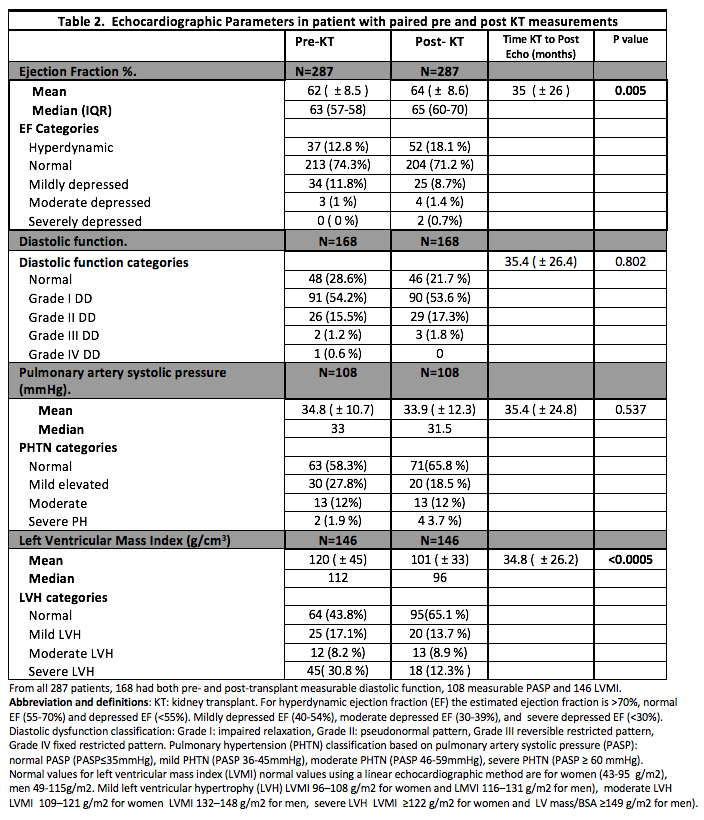
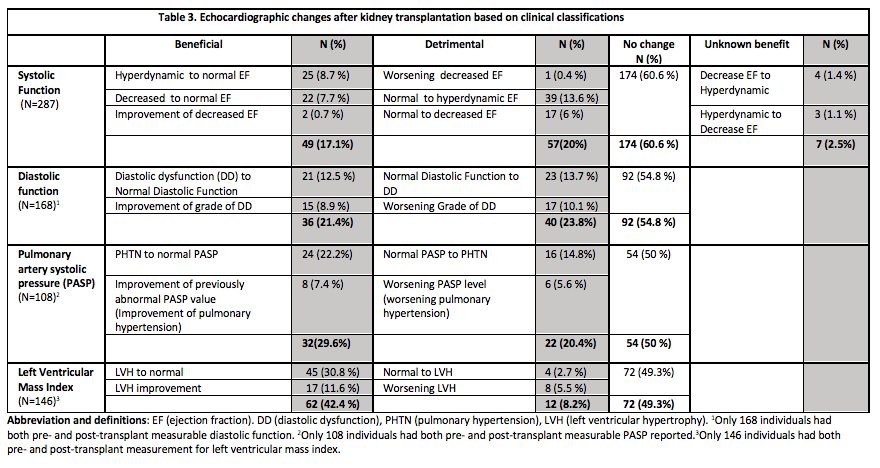
A greater proportion of patients had hyperdynamic EF (18.1%) post-KT compared to pre-KT (12.8%). 42% of patients had a beneficial change in LVMI post-KT through normalization of a previously hypertrophic state or improvement in LVH degree.
Hyperdynamic EF pre-KT was associated with a higher risk of transplant failure {HR=3.1, 95 % CI (1.4-6.8) p=0.006} vs. normal EF. Moderate and severely reduced EF post-KT was associated with an increased risk of death {HR=11.5, 95% CI (2.2-59.3) p=0.004} and {HR=24.9, 95% CI (2.4-258.2) p=0.007}, respectively compared to normal EF. Worsening EF after KT in patients with pre-existent low EF states was associated with an increased risk of mortality {HR=11.7, 95% CI (1.3-105.9) p=0.03}. Grade 4 DD before KT was associated with a higher risk of mortality {HR=22.3, 95%CI (1.2-412) p=0.034}. Improvement of the grade of pre-existent DD after KT was, unexpectedly, associated with a higher risk of death {HR=7.8, 95% CI (2.2-59.2) p=0.02}.
Conclusion: LVH regression was a common finding post-KT; conversely, variations on EF post-KT showed lack of overall benefit. EF >70 % was a predictor of graft loss before KT. Moreover, advanced pre-KT DD and low EF states after KT were predictors of mortality. More research is needed on whether strategies to mitigate detrimental cardiac changes can improve post-KT outcomes in this high-risk population.
[1] Pakfetrat M, Roozbeh J, Nikoo MH, Asem Z, Malekmakan L, Nikoo MA. Common echocardiography findings in pretransplant dialysis patients and their associations. Hong Kong J Nephrol. 2013;15(2):68-74. doi:10.1016/J.HKJN.2013.07.001
[2] Liefeldt L, Budde K. Risk factors for cardiovascular disease in renal transplant recipients and strategies to minimize risk. Transpl Int. 2010;23(12):1191-1204. doi:10.1111/j.1432-2277.2010.01159.x
[3] Souza FL de, Bezerra KB, Sousa AR, et al. Study of echocardiographic alterations in the first six months after kidney transplantation. Arq Bras Cardiol. 2012;98(6):505-513.
[4] Ślubowska K, Lichodziejewska B, Pruszczyk P, Szmidt J, Durlik M. Left Ventricular Hypertrophy in Renal Transplant Recipients in the First Year After Transplantation. Transplant Proc. 2014;46(8):2719-2723. doi:10.1016/j.transproceed.2014.08.019
[5] Abdelwhab S, Elshinnawy S. Pulmonary Hypertension in Chronic Renal Failure Patients. Am J Nephrol. 2008;28(6):990-997. doi:10.1159/000146076
[6] Wang SC, Garcia R, Torosoff M, et al. Influence of mildly and moderately elevated pulmonary artery systolic pressure on post-renal transplantation survival and graft function. Echocardiography. 2019;36(1):22-27. doi:10.1111/echo.14192
[7] Pilmore H, Dent H, Chang S, McDonald SP, Chadban SJ. Reduction in Cardiovascular Death After Kidney Transplantation. Transplantation. 2010;89(7):851-857.
[8] Navaneethan SD, Roy J, Tao K, et al. Prevalence, Predictors, and Outcomes of Pulmonary Hypertension in CKD. J Am Soc Nephrol. 2016;27(3):877-886
There are no comments yet...
