A multidisciplinary approach in the management of enteric hyperoxaluria in kidney transplant candidates and recipients
Matthew D'Costa1, Hatem Amer1, Brigid M. Amberg1, Jenniver L. Wells-Pittman1, Amanda R. Frodemann1, Melissa K. Gay1, Erin M. Dahlen1, Theresa I. Schnell1, Gwen M. Davidson1, Carol A. Nash1, Ted L. Mueller1, John C. Lieske1.
1Nephrology, Mayo Clinic, Rochester, MN, United States
Enteric Hyperoxaluria Working Group.
Introduction: Enteric hyperoxaluria (EH) can recur in the kidney allograft after transplantation which may lead to dysfunction and graft loss. Management is aimed at lowering oxalate in plasma (POx) and urine (UOx) by initiating a low fat, low oxalate diet as well as calcium supplements in increasing doses to bind dietary oxalate to achieve target levels. The aim of the study was to determine the feasibility, adherence, and outcomes of a multidisciplinary protocolized approach towards lowering POx and UOx in kidney transplant (KTx) candidates and recipients.
Methods: Based upon our standard practice we developed a nurse-driven protocol with input by nephrologists, registered nurses (RNs) and a dietician to manage ordering and monitoring POx and UOx (Figure 1).
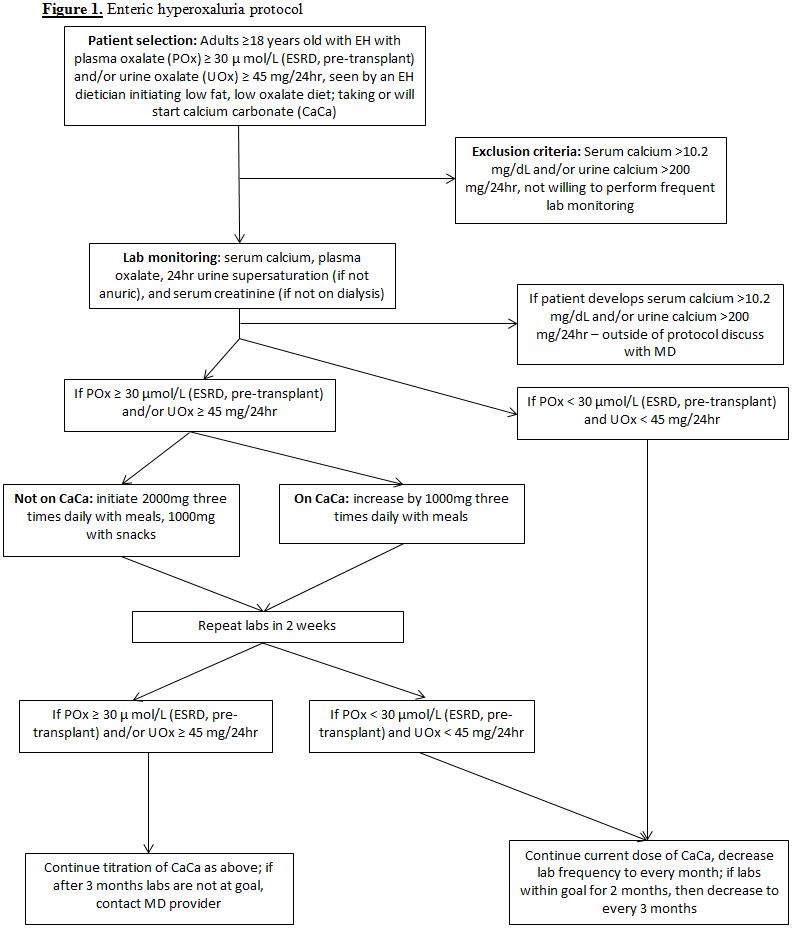
Once enrolled, EH KTx candidates were manages by an RN-nephrologist team for lab monitoring and medication titration. Patients were deferred for transplant until a POx concentration < 30 µmol/L was achieved. For each subject the study period was defined as from date of protocol enrollment until dismissal or 12/15/2019 (whichever occurred later). Outcomes included protocol adherence, achievement of a POx < 30 µmol/L and UOx < 45 mg/day at any point during follow-up prior to transplant, and adverse events. Among ultimate KTx recipients we assessed the incidence of delayed graft function (DGF), graft loss, new kidney stones, and oxalate deposition on protocol biopsies.
Results: After initiation of the EH protocol on 11/01/2015, 36 KTx candidates were enrolled of which 13 were ultimately transplanted. Baseline characteristics (Table 1) between ultimate recipients and non-recipients differed only by follow-up time.
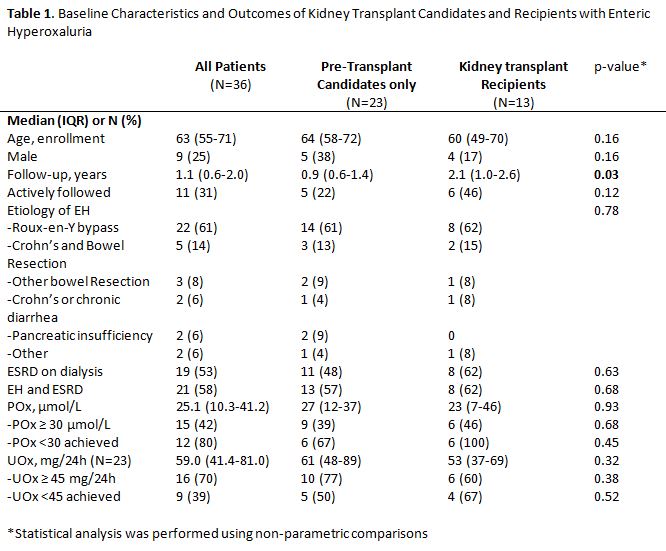
A total of 11 patients remain active. The most common reasons for dismissal (N=25) were nonadherence or loss to follow-up (N=6), provider specific management or resistance to the protocol (N=5), and adverse events (N=4) including hypercalcemia/ hypercalciuria (N=3) and calciphylaxis (N=1) that was attributed to inadequate dialysis. Goal POx was achieved in 80% of those with an initially elevated value including all KTx recipients prior to transplant. KTx recipients (12 living donor) had a median 0.7 (0.4-1.8) years post-transplant follow up. Only one DGF event occurred in a deceased donor recipient who also manifests numerous calcium oxalate crystals on a 1 year protocol biopsy. Of the remaining KTx recipients, two had rare calcium oxalate deposition on protocol biopsies with one additional recipient developing new stones attributed to hypocitraturia since they had a normal POx and UOx. All grafts were functioning at last follow-up.
Conclusion: This study demonstrated the feasibility of a nurse driven protocol to successfully lower POx and UOx in EH patients prior to KTx. While nonadherence was common, among the remainder POx and UOx achieved target and the protocol was well tolerated. Outcomes post-transplant are favorable especially in living donor recipients.
There are no comments yet...
