Pure laparoscopic versus open right hepatectomy in live liver donors: a propensity score matched analysis
Suk Kyun Hong1, Ming Yuan Tan1, Lapisatepun Worakitti1, Jeong-Moo Lee1, Jae-Hyung Cho1, Nam-Joon Yi1, Kwang-Woong Lee1, Kyung-Suk Suh1.
1Surgery, Seoul National University College of Medicine, Seoul, Korea
Background: Although PLDRH is gradually spreading worldwide, their outcomes including long-term outcomes of both donor and recipient have not yet been evaluated in a large comparative study. The aim of this study is to present the safety and feasibility of pure laparoscopic donor right hepatectomy (PLDRH) compared with that of conventional donor right hepatectomy (CDRH).
Methods: We retrospectively reviewed the medical records of 894 donors who underwent LDLT between January 2010 to September 2018 at Seoul National University Hospital were reviewed. We performed 1:1 propensity score matching between the PLDRH and CDRH groups. Subsequently, 198 donor and counter recipients were included in each group.
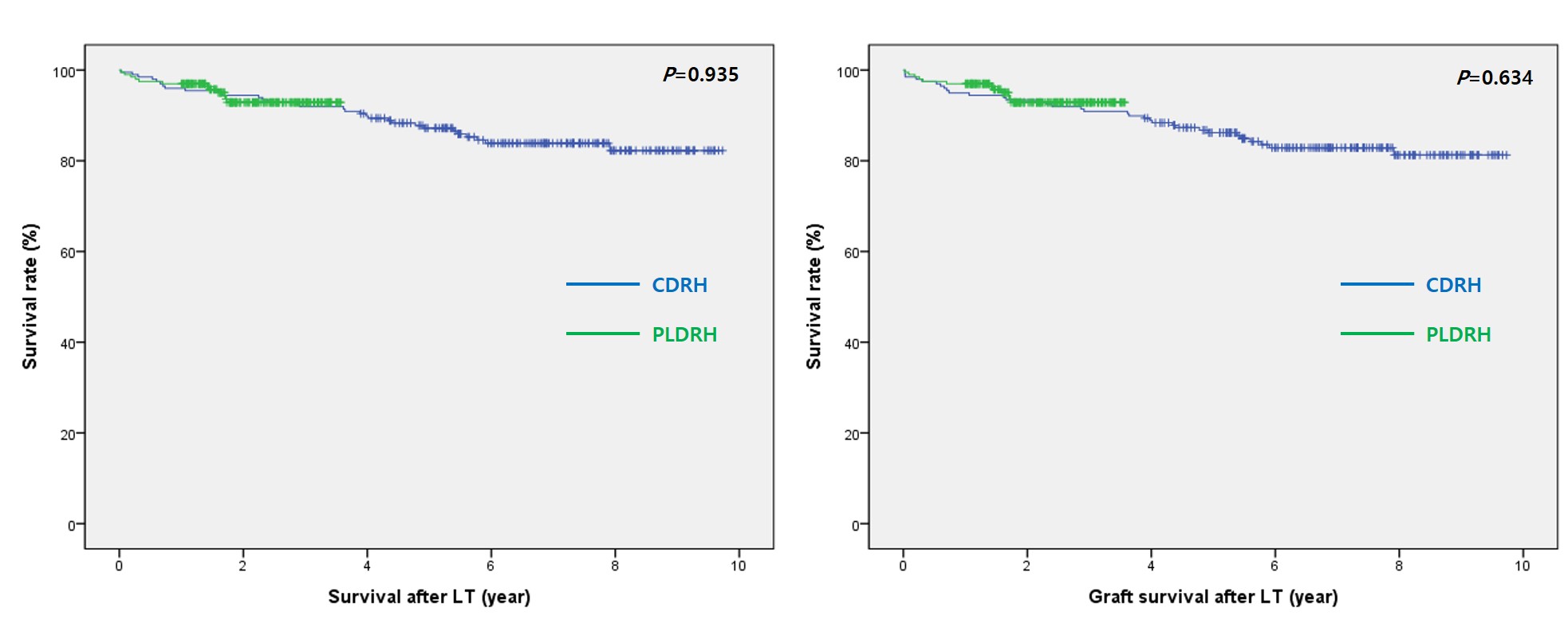
Results: The total operation time (P< 0.001), time to remove the liver (P< 0.001), and warm ischemic time (P< 0.001) were longer in the PLDRH group. The length of postoperative hospital stay was significantly shorter in the PLDRH group (P< 0.001). Although the rate of complication in donor was similar between the two groups, the rates of early (P=0.019) and late (P< 0.001) biliary complication in recipient were higher in PLDRH group. There was no significant difference in overall survival and graft survival between the two groups.
Conclusion: PLDRH is feasible when performed at an experienced LDLT center. Further studies on long-term recipient outcomes including biliary complications are needed to confirm the safety.
[1] Cherqui D, Soubrane O, Husson E, et al. Laparoscopic living donor hepatectomy for liver transplantation in children. Lancet. 2002;359:392–396.
[2] Troisi RI. Open or laparoscopic living donor liver hepatectomy: still a challenging operation! Am J Transplant. 2014;14:736.
[3] Troisi RI, Wojcicki M, Tomassini F, et al. Pure laparoscopic full-left living donor hepatectomy for calculated small-for-size LDLT in adults: proof of concept. Am J Transplant. 2013;13:2472–2478.
[4] Olivier S, Katsanos G, Olivier B, et al. Pure laparoscopic left lateral sectionectomy in living donors: from innovation to development in France. Ann Surg. 2015;261:506–512.
[5] Takahara T, Wakabayashi G, Nitta H, et al. The first comparative study of the perioperative outcomes between pure laparoscopic donor hepatectomy and laparoscopy-assisted donor hepatectomy in a single institution. Transplantation. 2017;101:1628–1636.
[6] Samstein B, Cherqui D, Rotellar F, et al. Totally laparoscopic full left hepatectomy for living donor liver transplantation in adolescents and adults. Am J Transplant. 2013;13:2462–2466.
[7] Rotellar F, Pardo F, Benito A, et al. Totally laparoscopic right hepatectomy for living donor liver transplantation: analysis of a preliminary experience on 5 consecutive cases. Transplantation. 2017;101:548–554.
[8] Han HS, Cho JY, Yoon YS, et al. Total laparoscopic living donor right hepatectomy. Surg Endosc. 2015;29:184.
[9] Kim KH, Kang SH, Jung DH, et al. Initial outcomes of pure laparoscopic living donor right hepatectomy in an experienced adult living donor liver transplant center. Transplantation. 2017;101:1106–1110.
[10] Kim KH, Jung DH, Park KM, et al. Comparison of open and laparoscopic live donor left lateral sectionectomy. Br J Surg. 2011;98:1302–1308.
[11] Suh KS, Hong SK, Lee KW, et al. Pure laparoscopic living donor hepatectomy: focus on 55 donors undergoing right hepatectomy. Am J Transplant. 2018;18:434–443.
[12] Hong SK, Lee KW, Choi Y, et al. Initial experience with purely laparoscopic living-donor right hepatectomy. Br J Surg. 2018;105:751–759.
[13] Buell JF, Cherqui D, Geller DA, et al. The international position on laparoscopic liver surgery: the Louisville Statement, 2008. Ann Surg. 2009;250:825–830.
[14] Wakabayashi G, Cherqui D, Geller DA, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg. 2015;261:619–629.
[15] Abu Hilal M, Aldrighetti L, Dagher I, et al. The Southampton consensus guidelines for laparoscopic liver surgery: from indication to implementation. Ann Surg. 2018;268:11–18.
[16] Nugroho A, Kim OK, Lee KW, et al. Evaluation of donor workups and exclusions in a single-center experience of living donor liver transplantation. Liver Transpl. 2017;23:614–624.
[17] Yi NJ, Suh KS, Suh SW, et al. Excellent outcome in 238 consecutive living donor liver transplantations using the right liver graft in a large volume single center. World J Surg. 2013;37:1419–1429.
[18] Yi NJ, Suh KS, Cho JY, et al. Three-quarters of right liver donors experienced postoperative complications. Liver Transpl. 2007;13:797–806.
[19] Suh KS, Suh SW, Lee JM, et al. Recent advancements in and views on the donor operation in living donor liver transplantation: a single-center study of 886 patients over 13 years. Liver Transpl. 2015;21:329–338.
[20] Lee KW, Hong SK, Suh KS, et al. One hundred and fifteen cases of pure laparoscopic living donor right hepatectomy at a single center. Transplantation. 2018;102:1878–1884.
[21] Suh KS, Kim SH, Kim SB, et al. Safety of right lobectomy in living donor liver transplantation. Liver Transpl. 2002;8:910–915.
[22] Hong SK, Lee KW, Kim HS, et al. Optimal bile duct division using real-time indocyanine green near-infrared fluorescence cholangiography during laparoscopic donor hepatectomy. Liver Transpl. 2017;23:847–852.
[23] Hong SK, Shin E, Lee KW, et al. Pure laparoscopic donor right hepatectomy: perspectives in manipulating a flexible scope. Surg Endosc. 2019;33:1667–1673.
[24] Hong SK, Suh KS, Kim HS, et al. Pure 3D laparoscopic living donor right hemihepatectomy in a donor with separate right posterior and right anterior hepatic ducts and portal veins. Surg Endosc. 2017;31:4834–4835.
[25] Hong SK, Suh KS, Lee JM, et al. New technique for management of separate right posterior and anterior portal veins in pure 3D laparoscopic living donor right hepatectomy. J Gastrointest Surg. 2019. Sep 4 [Epub ahead of print] DOI:10.1007/s11605-019-04350-6.
[26] Suh KS, Hong SK, Yi NJ, et al. Pure 3-dimensional laparoscopic extended right hepatectomy in a living donor. Liver Transpl. 2016;22:1431–1436.
[27] Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187–196.
[28] Soubrane O, Perdigao Cotta F, Scatton O. Pure laparoscopic right hepatectomy in a living donor. Am J Transplant. 2013;13:2467–2471.
[29] Rotellar F, Pardo F, Benito A, et al. Totally laparoscopic right-lobe hepatectomy for adult living donor liver transplantation: useful strategies to enhance safety. Am J Transplant. 2013;13:3269–3273.
[30] Han YS, Ha H, Han JR, et al. ABO incompatible living donor liver transplantation using dual grafts and pure laparoscopic donor right hepatectomy: a case report. Medicine (Baltimore). 2018;97:e13639.
[31] Rhu J, Choi GS, Kim JM, et al. Intraoperative ultrasonography as a guidance for dividing bile duct during laparoscopic living donor hepatectomy. Ann Transplant. 2019;24:115–122.
[32] Kwon CHD, Choi GS, Joh JW. Laparoscopic right hepatectomy for living donor. Curr Opin Organ Transplant. 2019;24:167–174.
[33] Park J, Kwon DCH, Choi GS, et al. Safety and risk factors of pure laparoscopic living donor right hepatectomy. Transplantation. 2019;103:e308–e316.
[34] Park J, Kwon CHD, Choi GS, et al. One-year recipient morbidity of liver transplantation using pure laparoscopic versus open living donor right hepatectomy: propensity score analysis. Liver Transpl. 2019;25:1642–1650.
[35] Au KP, Chok KSH. Minimally invasive donor hepatectomy, are we ready for prime time? World J Gastroenterol. 2018;24:2698–2709.
[36] Hong SK, Lee KW, Yi NJ, et al. Pure laparoscopic donor right hepatectomy: brightening the dark side of the moon in the era of space travel. Laparosc Surg. 2018;2:67–69.
[37] Hong SK, Suh KS, Yoon KC, et al. The learning curve in pure laparoscopic donor right hepatectomy: a cumulative sum analysis. Surg Endosc. 2019;33:3741–3748.
[38] Samstein B, Griesemer A, Halazun K, et al. Pure laparoscopic donor hepatectomies: ready for widespread adoption? Ann Surg. 2018;268:602–609.
[39] Song JL, Yang J, Wu H, et al. Pure laparoscopic right hepatectomy of living donor is feasible and safe: a preliminary comparative study in China. Surg Endosc. 2018;32:4614–4623.
[40] Lentsch AB, Yoshidome H, Kato A, et al. Requirement for interleukin-12 in the pathogenesis of warm hepatic ischemia/reperfusion injury in mice. Hepatology. 1999;30:1448–1453.
[41] Hong JC, Yersiz H, Kositamongkol P, et al. Liver transplantation using organ donation after cardiac death: a clinical predictive index for graft failure-free survival. Arch Surg. 2011;146:1017–1023.
[42] Wang MF, Jin ZK, Chen DZ, et al. Risk factors of severe ischemic biliary complications after liver transplantation. Hepatobiliary Pancreat Dis Int. 2011;10:374–379.
[43] Olthof PB, van Golen RF, Meijer B, et al. Warm ischemia time-dependent variation in liver damage, inflammation, and function in hepatic ischemia/reperfusion injury. Biochim Biophys Acta Mol Basis Dis. 2017;1863:375–385.
[44] Singal R, Singal RP, Sandhu K, et al. Evaluation and comparison of postoperative levels of serum bilirubin, serum transaminases and alkaline phosphatase in laparoscopic cholecystectomy versus open cholecystectomy. J Gastrointest Oncol. 2015;6:479–486.
[45] Xu GS, Liu HN, Li J, et al. Hepatic injury induced by carbon dioxide pneumoperitoneum in experimental rats. World J Gastroenterol. 2009;15:3060–3064.
[46] Ishizawa T, Bandai Y, Ijichi M, et al. Fluorescent cholangiography illuminating the biliary tree during laparoscopic cholecystectomy. Br J Surg. 2010;97:1369–1377.
[47] Park CS, Jung BH, Hwang S, et al. External biliary drainage in living donor liver transplantation using duct-to-duct anastomosis. Transplant Proc. 2014;46:678–681.
There are no comments yet...