Visual rehabilitation after penetrating keratoplasty
Leyla Asena1, Dilek Dursun Altınors1, Sibel Oto1.
1Ophthalmology, Baskent University Faculty of Medicine, Ankara, Turkey
Introduction: Astigmatism is the most common cause of suboptimal vision after corneal transplantation despite a clear corneal graft.1
Based on several studies, 15–31% of patients undergoing penetrating keratoplasty (PK) may develop postoperative astigmatism greater than 5 diopters (D).2,3
Commonly practiced techniques for visual rehabilitation after PK consist of postoperative suture manipulation, optical correction consisting of spectacles and contact lenses, relaxing incisions, compression sutures, laser refractive surgery, insertion of intrastromal corneal ring segments, wedge resection, toric phakic intraocular lenses, and finally regrafting.4
The aim of this study was to report our management strategies and their results performed for visual rehabilitation and management of astigmatism after PK.
Patients and Methods: The records of 104 eyes of 98 patients (54male/44 female) who underwent PK between January 2013 and January 2015 in Baskent University Faculty of Medicine, Department of Ophthalmology were reviewed.
The age, the indication for PK, interventions performed for visual rehabilitation, the duration of follow-up, the topographic and refractive astigmatism at the end of follow-up and the final BCVA were recorded.
Results: The mean age of the patients was 54±23 years.
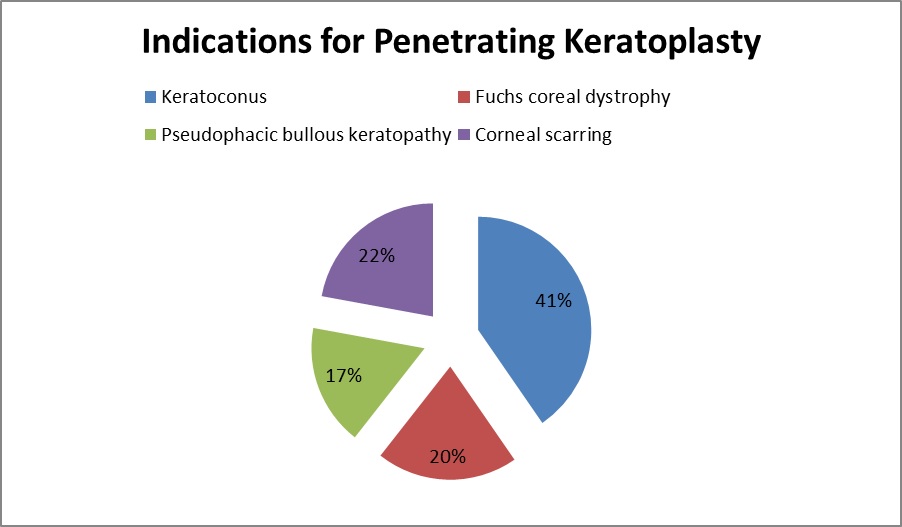
The indications for PK included keratoconus, Fuch's endothelial dystrophy, pseudophakic bullous keratopathy and corneal scarring (Figure 1).
The mean duration of follow up was 23±11.5 months.
Suture adjustment and selective suture removal were performed 2 to 6 weeks and after 3 months in eyes with more than 3 D of corneal astigmatism.
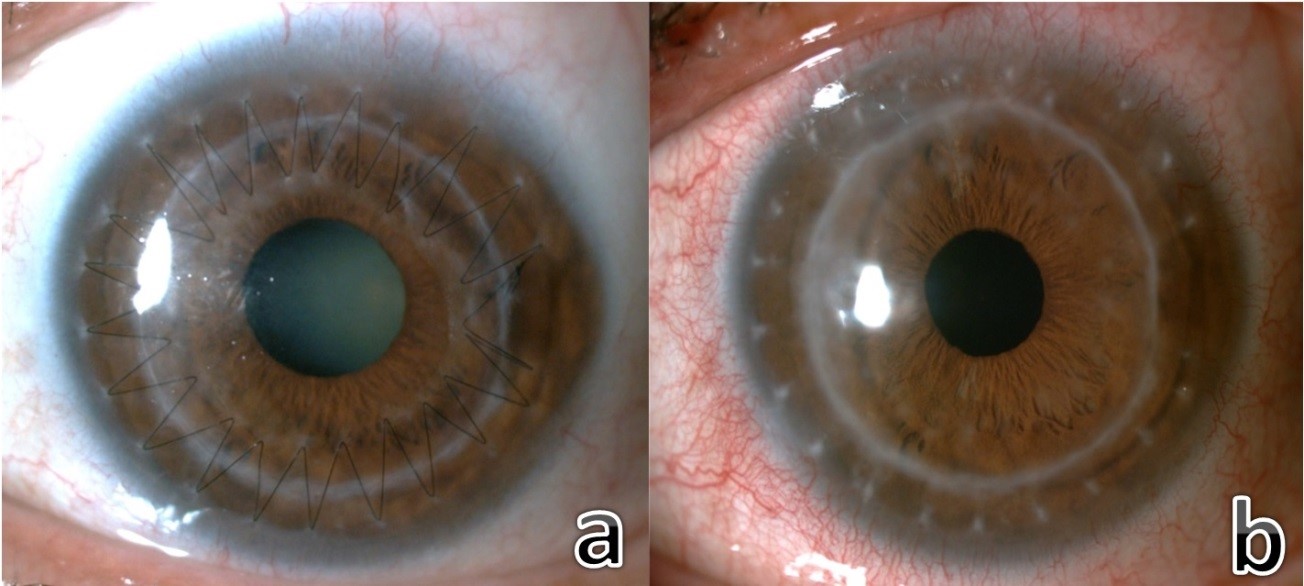
Spectacle correction was performed in 86 eyes (83%) and contact lenses including rigid gas permeable and scleral lenses were fitted in 18 eyes (17%) who were unsatisfied with spectacle correction mostly due to higher order aberrations or high anisometropia (Figure 2).
Relaxing corneal incisions were performed in 23 eyes (22%) and toric intraocular lens implantation was performed in 34 eyes (33%) with cataracts.
The mean topographic and absolute refractive astigmatism at the end of follow up was 3.4±2.6 D and 3.6± 1.9 D, respectively.
Discussion: Intraoperative and postoperative suture manipulation have been described for minimising early postoperative astigmatism.5,6
After PK, sutures should be kept for at least one year. During this period, astigmatism >4 D can be reduced by suture manipulation consisting of selective interrupted suture removal and tension adjustment of running sutures.4
If significant astigmatism remains after suture removal, which cannot be corrected by optical means such as spectacle correction or contact lenses, surgical procedures can be performed.4
Conclusion: Although general guidelines are useful, it is important to individualize the management based on corneal topography and patient expectations for successful visual rehabilitation.
[1] Price NC. Steele AD. The correction of postkeratoplasty astigmatism. Eye 1987; 1(5): 562–566.
[2] Williams KA, Roder D, Esterman A, Muehlberg SM, Coster DJ. Factors predictive of corneal graft survival: report from the Australian corneal graft registry. Ophthalmology. 1992 Mar;99(3):403-14.
[3] Olson RJ, Pingree M, Ridges R, Lundergan ML, Alldredge C Jr, Clinch TE. Penetrating keratoplasty for keratoconus: a long-term review of results and complications. J Cataract Refract Surg. 2000 Jul;26(7):987-91.
[4] Feizi S, Zare M. Current approaches for management of postpenetrating keratoplasty astigmatism. J Ophthalmol. 2011;2011:708736.
[5] Küçükerdönmez C, Akova YA, Dursun D. Refractive outcome of single running suture adjustment in penetrating keratoplasty. Eur J Ophthalmol. 2004 Mar-Apr;14(2):94-9.
[6] Dursun D, Forster RK, Feuer WJ. Surgical technique for control of postkeratoplasty myopia, astigmatism, and anisometropia. Am J Ophthalmol. 2003 Jun;135(6):807-15.
There are no comments yet...