Limbal stem cell transplantation for restoration of the ocular surface health in bilateral limbal stem cell deficiency
Dilek Dursun Altınors1, Leyla Asena1, Sibel Oto1.
1Ophthalmology, Baskent University Faculty of Medicine, Ankara, Turkey
Introduction: Limbal stem cell deficiency (LSCD) may ocur secondary to severe dry eye, chronic inflammation of the ocular surface, chemical burns, Stevens Johnsons Syndrome or may be due to congenital reasons such as in congenital aniridia. Corneal transplantation alone is unsuccesfull in limbal deficient recipients and has to be combined with limbal stem cell transplantation (LSCT) for an optimum outcome. Surgical treatment in LSCD can be performed contralateral conjunctival limbal autograft transplantation in unilateral cases. In bilateral cases, keratolimbal allograft procedure from a cadaveric source coupled with systemic immunosuppression or limbal allograft taken from a living related donor who is HLA compatible can be performed.1 Here, we report the results of LSCT in patients with bilateral LSCD.
Patients and Methods: Six patients (3M/FM) with bilateral limbal stem cell deficiency were treated in Baskent Univesity Faculty of Medicine, Department of Ophthalmology between December 2017 and March 2019. Living-related conjunctival allograft (Ir-CAL) transplantation was performed in 3 cases and cadaveric keratolimbal allograft (KLAL) transplantation was performed in 3 cases.
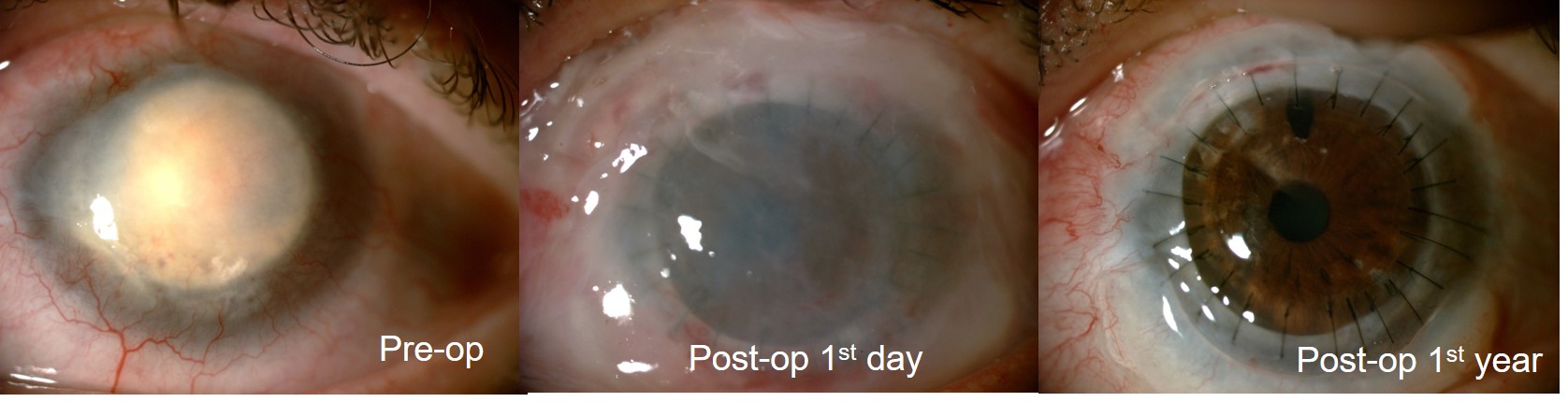
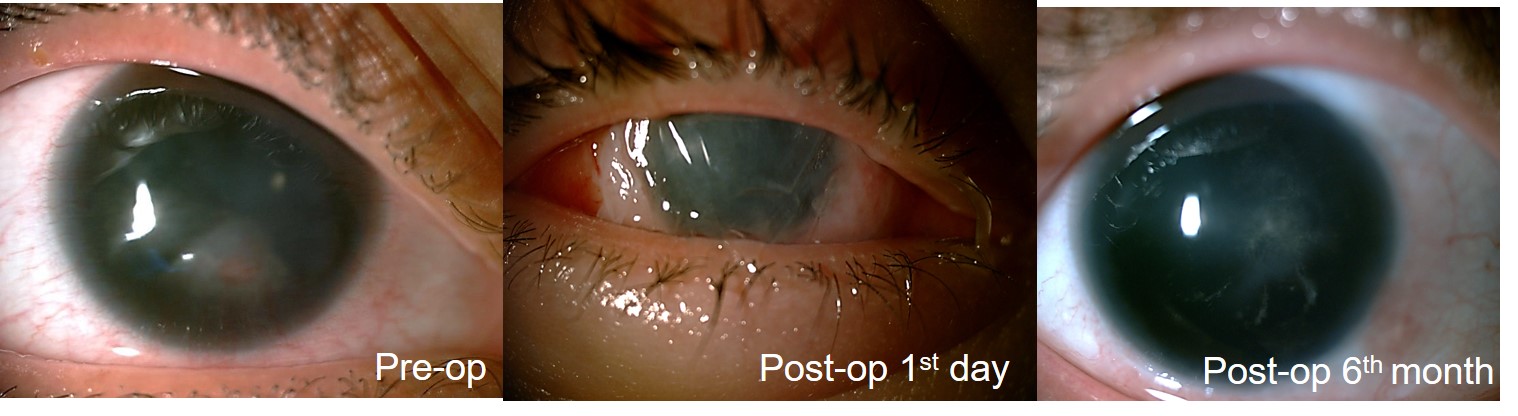
Results: The mean age of the patients was 33.8±13.8 years (range; 14-46 years). The etiology of bilateral LSCD was Sjögrens’ Syndrome in 1 patient, Steven Johnsons Syndrome in 1 patient, chemical injury (alkali burn) in 2 patients and congenital aniridia in 2 patients. The mean duration of preoperative follow-up was 13.3±8.1 months. Visual acuity increased in all patients except in one case who developed fungal keratitis 2 months after KLAL transplantation. All patients were given systemic 1-1.5 mg/kg Cyclosporin A postoperatively for prevention of a rejection reaction. The mean postoperative follow up duration was 25.8±16.6 months. Corneal transplantation was performed simultaniously in 4 patients and, 1 and 2 years after LSCT in two other patients. Simultaneous amniotic membrane transplantation (AMT) was performed in 3 patients. Figure 1 and 2 show pre- and postoperative anterior segment photographs of a patient who underwent cadaveric KLAL transplantation + PKP +AMT for alkali burn and living-related conjunctival allograft transplantation + AMT in another patient with congenital aniridia, respectively.
Discussion: Treatment and restoration of the ocular surface health is challenging in bilateral LSCD. Tissue engineering or newer tissue culturing techniques are bound to play a significant role in the future because the goal is to develop nonimmunogenic tissues that decrease or eliminate the need for systemic immunosuppression. In the future, more refined treatment options such as transplantation of cultivated limbal epithelial cells might be available.2,3
Conclusion: Living-related conjunctival allograft transplantation and cadaveric keratolimbal allograft transplantation are currently available surgical techniques in patients with bilateral LSCD.
[1] Vazirani J, Mariappan I, Ramamurthy S, Fatima S, Basu S, Sangwan VS.Surgical Management of Bilateral Limbal Stem Cell Deficiency. Ocul Surf. 2016 Jul;14(3):350-64.
[2] Dong Y, Peng H, Lavker RM. Emerging Therapeutic Strategies for Limbal Stem Cell Deficiency. J Ophthalmol. 2018 Jun 27;2018:7894647.
[3] Sangwan VS, Murthy SI, Vemuganti GK,et al. Cultivated corneal epithelial transplantation for severe ocular surface disease in vernal keratoconjunctivitis.
There are no comments yet...