Removing the BMI bias in kidney transplantation: Outcomes of kidney transplantation in patients with BMI >35
Aaron Hui1, Nancy Suh1, Matthew Sypek2.
1General and Renovascular Surgery, The Royal Melbourne Hospital, Melbourne, Australia; 2Department of Nephrology, The Royal Melbourne Hospital, Melbourne, Australia
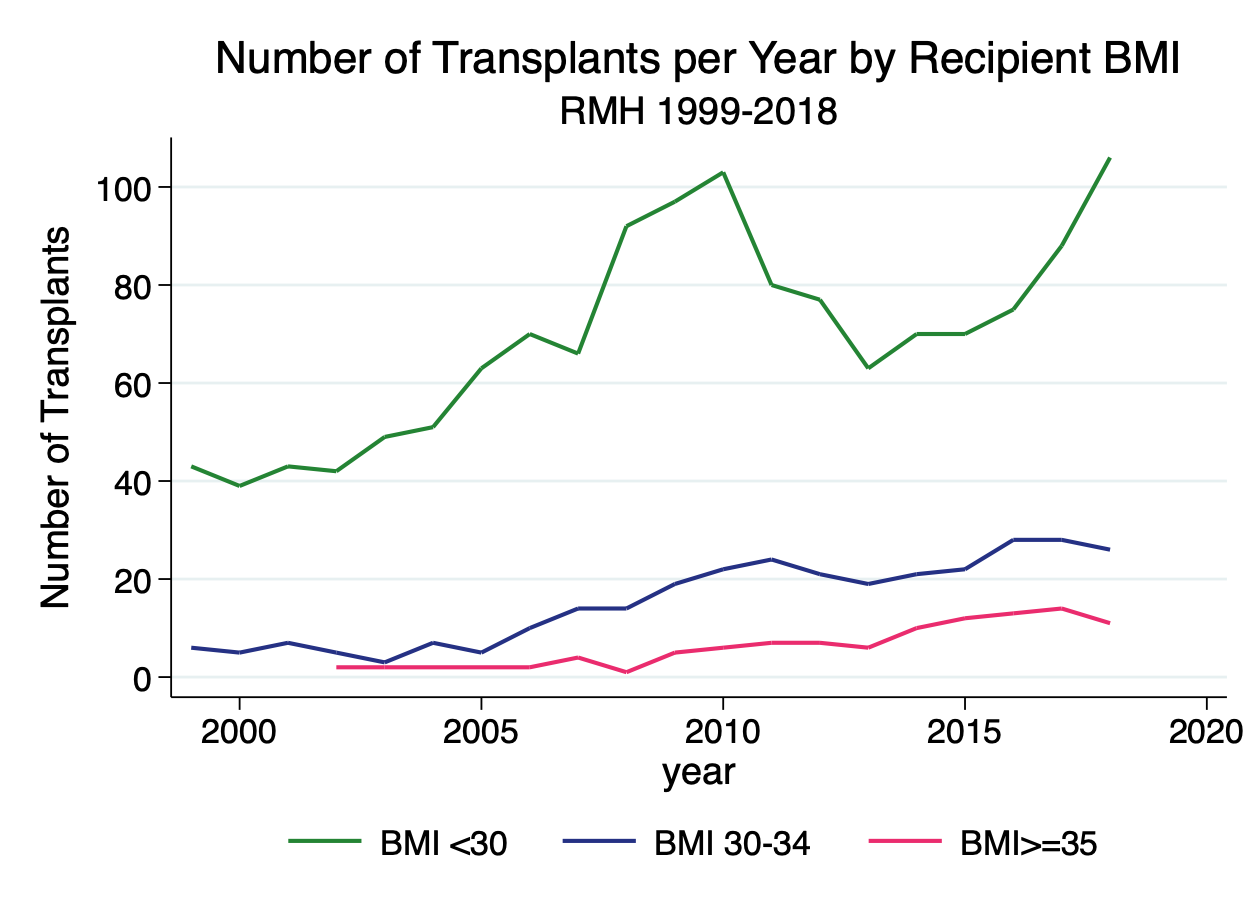
Background: Body Mass Index (BMI) is often used a surrogate marker of suitability for kidney transplantation1,2. Some centres in Australia will limit patients being waitlisted for transplantation unless there BMI is less than 35. With BMI increasing in the general population and the ever increasing diabetic and obesity related health issues such as renal failure, transplantation on patients with high BMI is inevitable3.
Methods: We used local and national data to retrospectively evaluate the outcomes of all patients that received a kidney transplant with a BMI > 35 pre-transplantation. Recipients that had undergone transplantation in the period of 2009-2018 with a BMI of 35 were compared against patients with a BMI of 31-34 and of BMI < 30. Graft function and overall survival was analysed using a univariate COX PH model and demonstrated with Kaplein-Meier curves, along with individual assessment of specific surgical complications.
Results: Of the 1222 renal transplants that were performed 102 patients had a BMI >35 with the overall survival and graft survival comparable to the BMI < 30 group. Median follow-up was 15.2 years. There was a slightly higher wound complication rate when compared to patients with a BMI < 30 (0.5% versus < 0.5%) P< 0.05. Cox model analysis showed no significant increase in hazards for BMI > 35 compared to BMI <30, but patients with BMI 31-34 had both increased hazards for both graft loss and death. Significant complications in the BMI >35 included a single mortality caused by a PE.
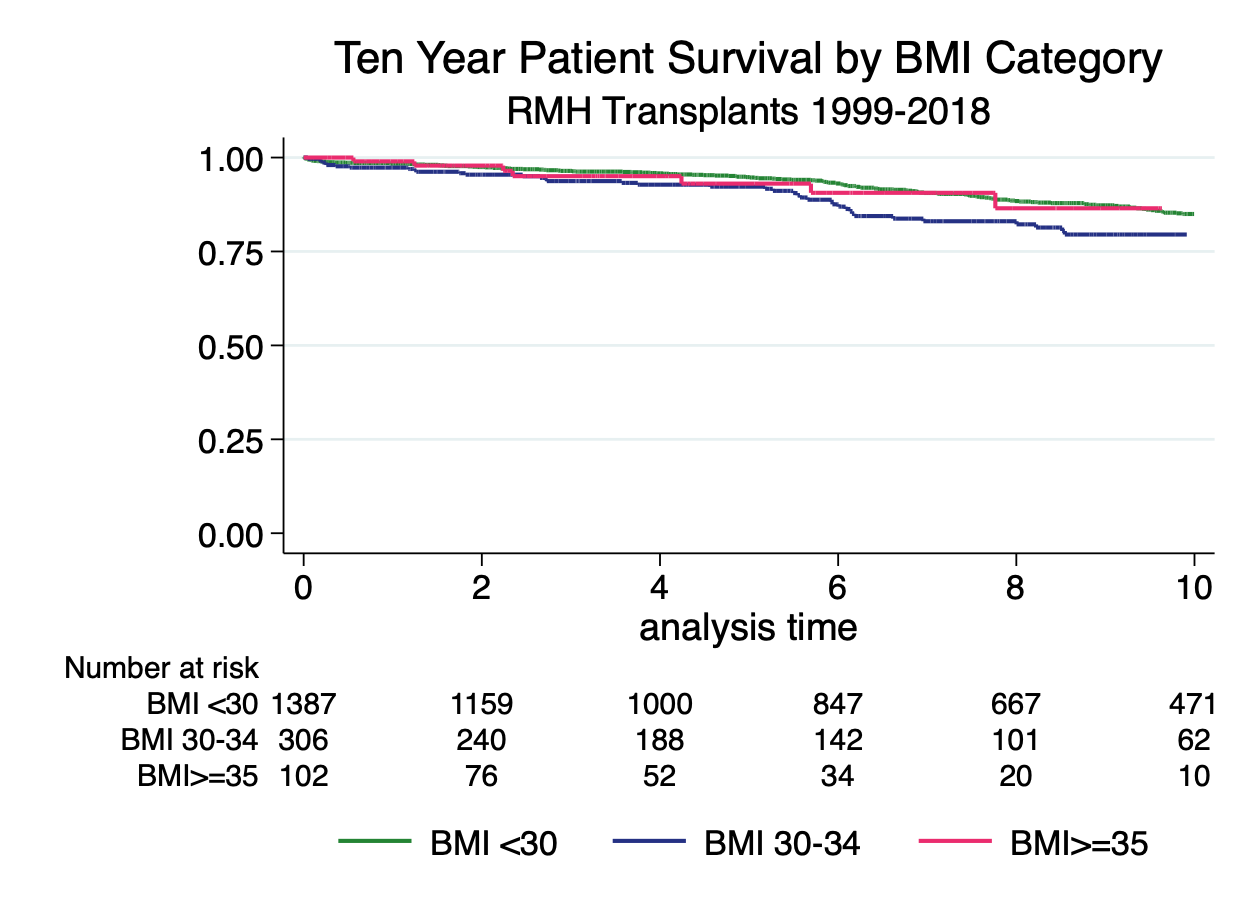
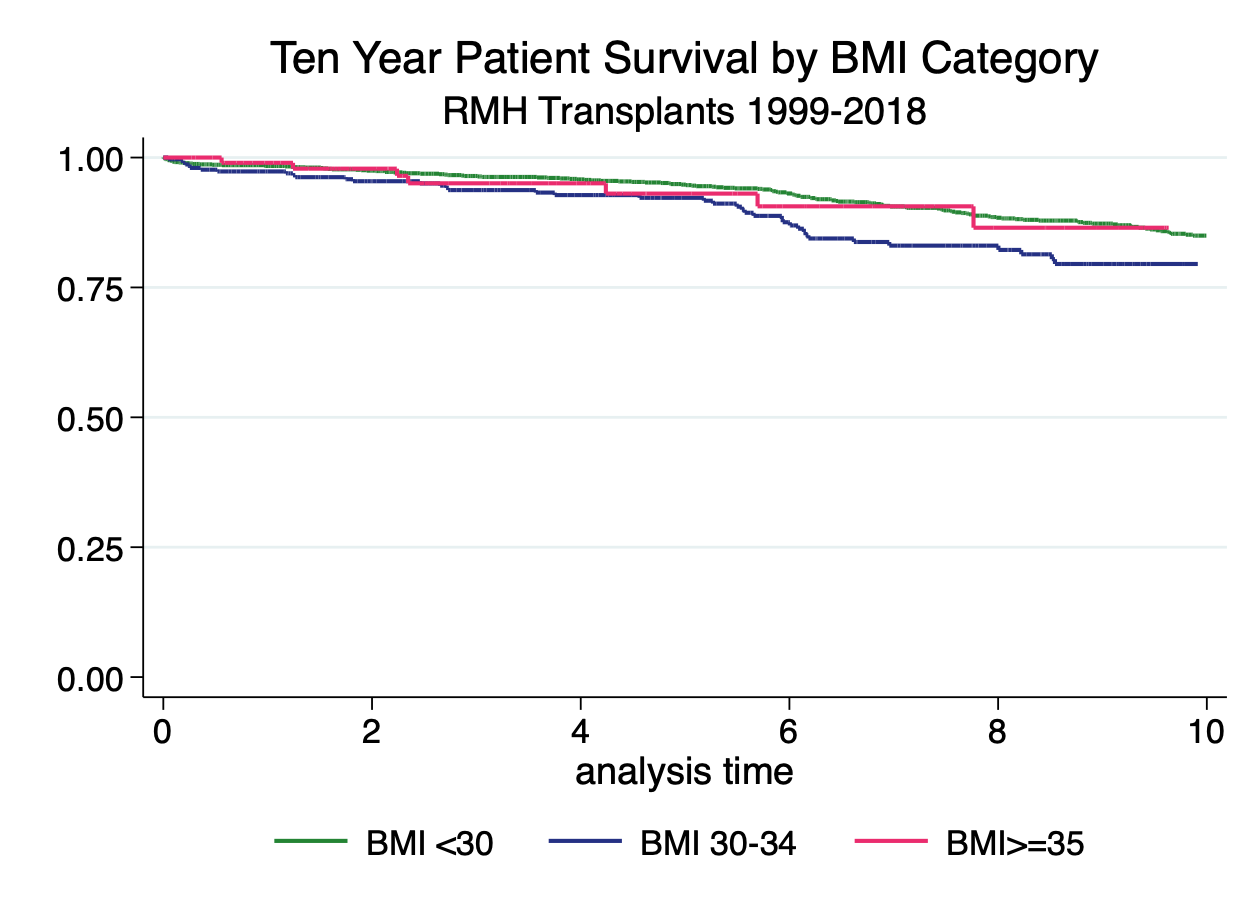
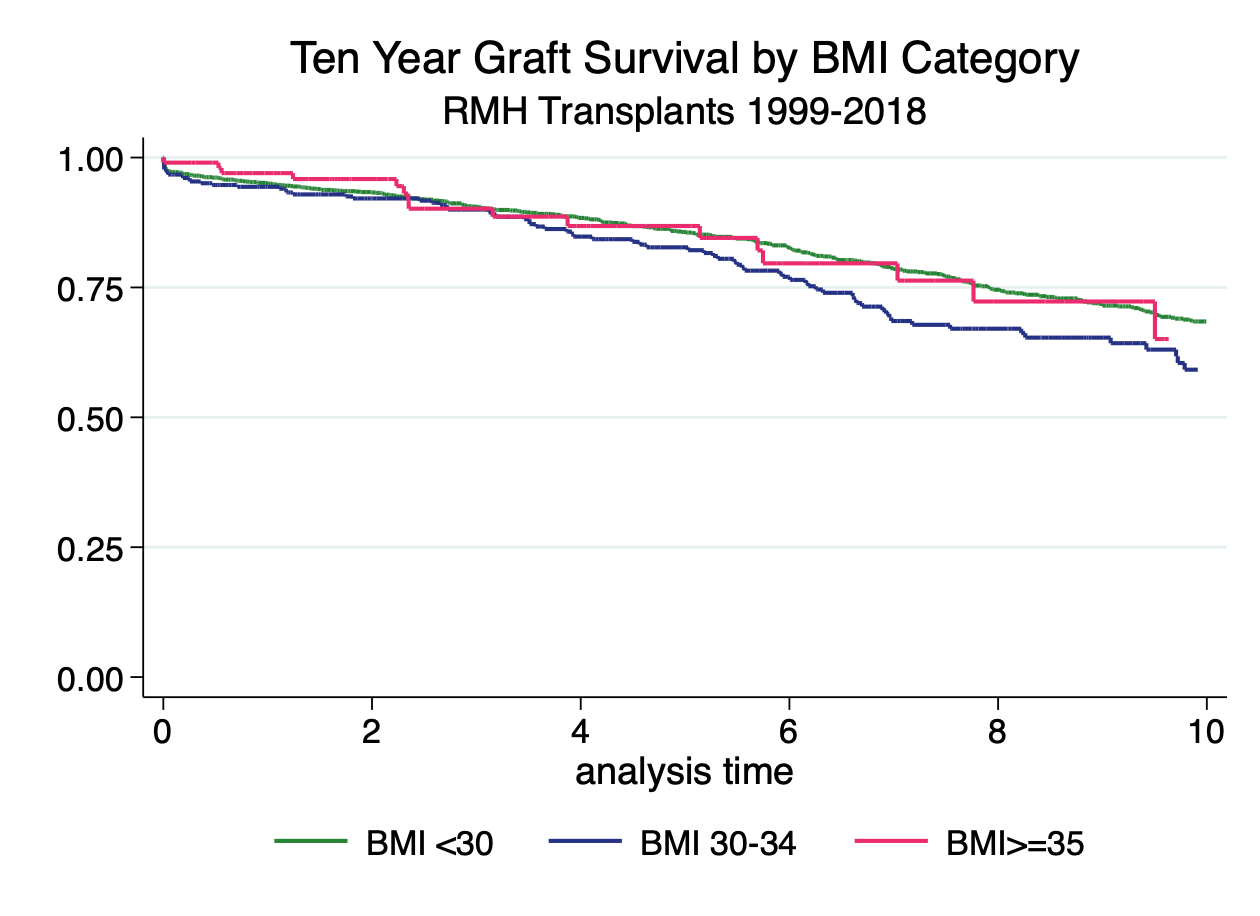
Discussion: It is well documented that there is an increased risk of surgical complications with kidney transplantation in the morbidly obese population, however this study raises the question of whether we should be using BMI as a marker for waitlist exclusion in Australia4,5. BMI does not account for issues with central adiposity that may make surgery more difficult and therefore more prone to complication 6,7,8. We beleive the slight rise in hazards for both graft loss and death in the BMI 31-34 group can be explained by more caution in the BMI > 35 population therefore reducing the co-morbid burden in this group. Obese patients may also be subject to closer clinical monitoring of other medical conditions and therefore receive greater medical input throughout their time on the transplant waiting list also influencing their outcomes post transplantation9,10,11. This study suggests that more caution should be undertaken in assessing patients with a BMI >35 and their suitability for transplantation particular in association with other medical co-morbidties.
Conclusion: This study highlights the need to re-evaluate the use of BMI in transplant assessment and may help to eliminate the BMI bias in waitlisting patients for kidney transplant, BMI > 35 patients should be a more highly selected population with a lower co-morbid burden.
[1] 2. Chan et al. the Impact and treatment of obesity in kidney transplant candidates and recipients. Canadian Journal of Kidney Health and Disease (2015) 2:26
[2] 3. Lassalle M, Fezeu LK, Couchoud C, Hannedouche T, Massy ZA, Czernichow S (2017) Obesity and access to kidney transplantation in patients starting dialysis: A prospective cohort study. PLoS ONE 12(5): e0176616
[3] 4. P Kanthawar, M Xiaonan, M Daily, J Chandarana, M Salah, J Berger, A.L Castellanos, F Marti, R Gedaly. Kidney transplant outcomes in the Super Obese: A National Study from the UNOS dataset. World J Surg (2016) 40:2802-2815
[4] 5. K Kaur & D Jun et al. Outcomes of underweight, overweight, and obese pediatric kidney transplant recipients. Pediatric Nephrology 2018) 33:2353-2362
[5] 6. J Liese et. al. Influence of the recipient body mass index on the outcomes after kidney transplantation; Langenbecks Arch Surg (2018) 403: 73-82
[6] 7. O.M McCloskey, P.A. Device, A.E. Courtney and J.A McCaughan. Is big bad or bearable? Long-term renal transplant outcomes in obese recipients. QJM: An International Journal of Medicine (2018) 365-371.
[7] 8. Alexander Mehta et al Where to draw the line in surgical obesity for renal transplantation Recipients: An Outcome analysis based on Body mass IndexExperimental and Clinical Transplantation (2019) 1: 37-41
[8] 9. Anne-Elisabeth Heng et al, Renal Transplant in Obese Patient and Impact of Weight Loss before Surgery on Surgical and Medical Outcomes: A Single- Center Cohort Study. Experimental and Clinical Transplantation (2018)
[9] 10. W Pommer. Preventive Nephrology: The role of chronic obesity in different stages of chronic kidney disease (2018) Kidney disease 4:199-204
[10] 12. Glanton C, Kao T, Cruess D, Agodoa L, Abbott K (2003) Impact of renal transplantation on survival in end-stage renal disease patients with elevated body mass index. Kidney Int 63(2):647–653
[11] 11. M Tran, C Foster, K Kalantar-Zadeh, H Ichii, Kidney transplantation in obese patients. World J Transplant 2016 March 24; 6(1): 135-143
There are no comments yet...