Pancreas transplant in chronic kidney disease for type 1 diabetic patients
Rashikh Choudhury1, Dor Yoeli1, Hunter B. Moore1, Hillary Yaffe1, Trevor L. Nydam1, Peter Kennealey1.
1Department of Surgery-Division of Transplantation Surgery, University of Colorado Hospital, Aurora, CO, United States
Background: Although both pancreas transplantation alone (PTA) and islet cell transplantation (ICT) have been associated with peri-operative declines in eGFR, the magnitude of decline is far less than that associated with medically managed (MM) diabetes. In the long-term, PTA and ICT have demonstrated stabilization of chronic kidney disease (CKD) for type 1 diabetic patients. In this setting, it remains unclear whether transplantation reduces future need for kidney transplantation and mortality.
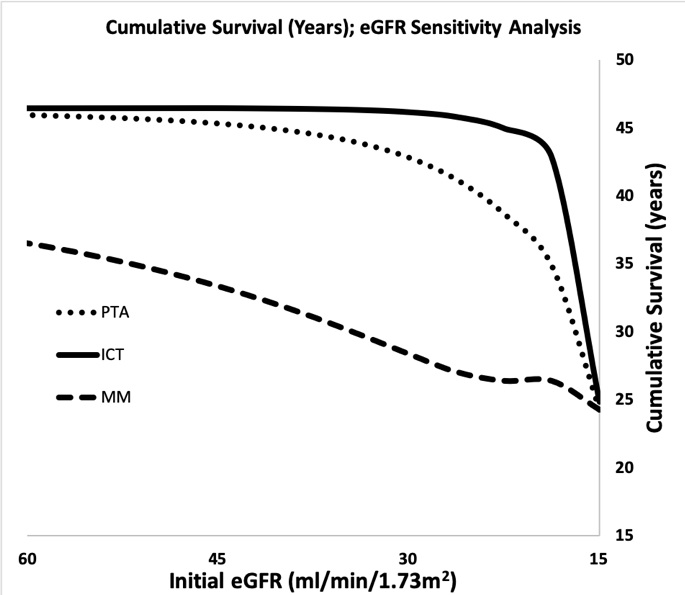
Methods: A decision analytic Markov state transition model was created to simulate the life of type 1 diabetic patients with CKD who underwent one of three interventions: 1) PTA, 2) ICT, or 3) MM. Estimated declines in eGFR, chance of requiring kidney transplant, and mortality were estimated following each intervention for a simulated cohort of 3,000 patients. Base case patients were defined as 30 year old type 1 diabetic patients with an initial eGFR of 30 ml/min/1.732. Sensitivity analysis of initial eGFR was performed. Markov model parameters were extracted from literature review (1-4).
Results: PTA and ICT was associated with improved long-term survival across a spectrum of initial eGRF (15-60 ml/min/1.732). For base case patients, ICT patients required few transplants, and gained 17.8 years of life compared to MM patients, and 3.8 years of life compared to PTA patients.
Conclusion: ICT is associated with stabilization of eGFR, thereby reducing need to future kidney transplantation and improving long-term survival.
[1] Perit Dial Int. 2019 Jan-Feb;39(1):25-34. doi: 10.3747/pdi.2017.00207.
[2] Transpl Int. 2019 Nov 9. doi: 10.1111/tri.13552
[3] World J Transplant. 2019 Aug 26;9(4):81-93. doi: 10.5500/wjt.v9.i4.81.
[4] Diabet Med. 2019 Nov 8. doi: 10.1111/dme.14177.
There are no comments yet...