Increased development of microthrombi and fibrin depositions in deceased donor kidney transplantation
Tamar AJ van den Berg1,2, Marius C. van den Heuvel3, Janneke Wiersema-Buist1,2, Jelle Adelmeijer1,2, Gertrude J. Nieuwenhuijs-Moeke4, Stephan JL Bakker5, Ton Lisman1,2, Harry van Goor3, Robert A. Pol1.
1Surgery, University Medical Center Groningen, Groningen, Netherlands; 2Surgical Research Laboratory, University Medical Center Groningen, Groningen, Netherlands; 3Pathology, University Medical Center Groningen, Groningen, Netherlands; 4Anesthesiology, University Medical Center Groningen, Groningen, Netherlands; 5Nephrology, University Medical Center Groningen, Groningen, Netherlands
Dutch Kidney Transplant Study Group (DKTSG).
In kidney transplantation, development of microthrombi(MT) and fibrin depositions in peritubular capillaries(PTC) and glomeruli, may potentially lead to local perfusion disorders, and subsequently to deterioration of graft function. The MT incidence, time of development, and association with different donor types or intraoperative heparinization of the recipient remained unclear.
To investigate this, two open-needle biopsies, pre-anastomosis and post reperfusion, were obtained from 43 kidneys transplanted from 2005 to 2008. Paraffin-embedded sections were immunohistochemically stained with an anti-fibrinogen antibody. MT/mm2 were scored by a trained nephropathologist and fibrin deposition intensity was categorized as negative, weak, moderate or strong.
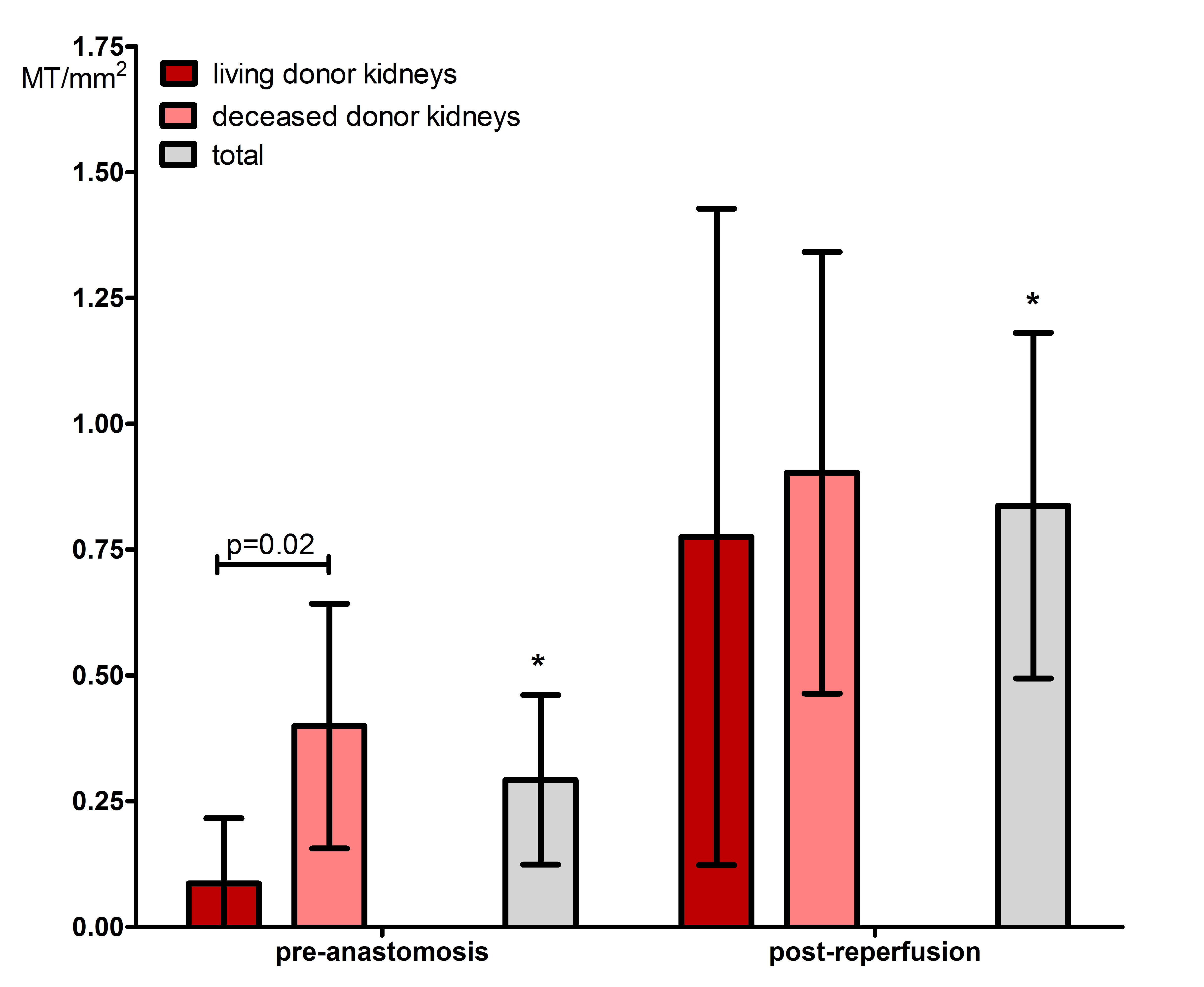
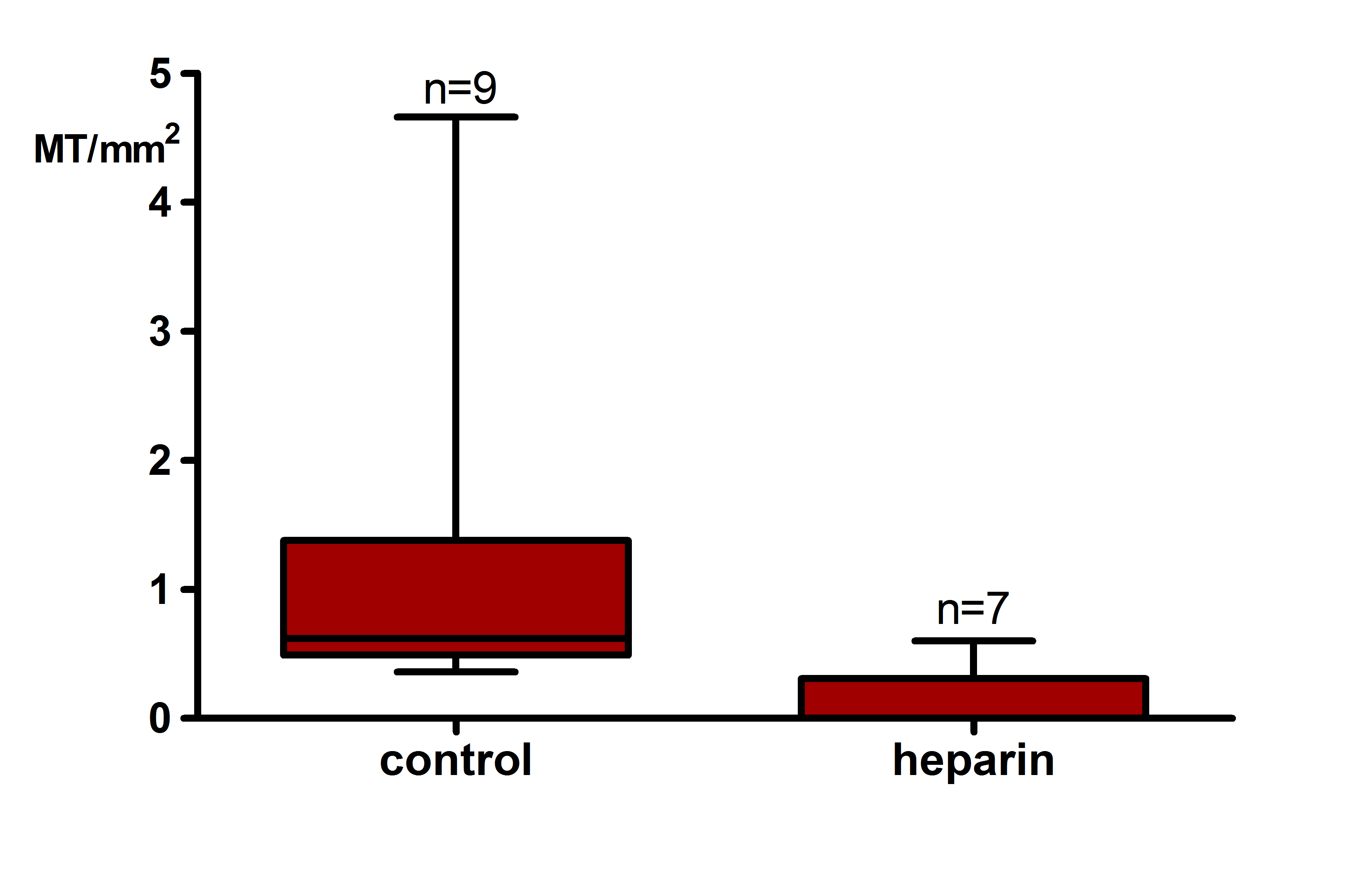
A significant increase in MT/mm2 (0.45[0–1.21] vs. 0[0–0.45], p<0.01. Figure 1) and generalized fibrin deposition (100% vs. 20% moderate/strong) was observed in postreperfusion biopsies compared to pre-anastomosis biopsies. Deceased donor kidneys showed significantly more MT/mm2 (0.09[0–0.66] vs. 0.00[0–0], p=0.02) and stronger fibrin intensity in glomeruli (28% vs. 0%, p<0.01) and PTC (14% vs. 0%, p=0.02) compared to living donor kidneys pre-anastomosis. Heparin infusion prior to reperfusion significantly reduced the number of MT/mm2 (0.62[0.49-1.38] vs. 0[0-0.31], p<0.01. Figure 2).
In conclusion, MT and a generalized deposition of fibrin in PTC and glomeruli develop during kidney transplantation. Deceased donor kidneys are more prone to this development. There may be a role for prophylactic heparinization of the recipient to inhibit this process.
There are no comments yet...