Reassessment of the relevance and predictive value of parameters indicating early graft dysfunction in liver transplantation: A retrospective single center experience
Margot Fodor1, Adriana Woerdenhoff1, Wolfgang Peter1, Hannah Esser1, Christian Margreiter1, Manuel Maglione1, Rupert Oberhuber1, Benno Cardini1, Heinz Zoller2, Herbert Tilg2, Dietmar Öfner1, Stefan Schneeberger1.
1Department of Visceral-Transplantation and Thoracic Surgery, Medical University of Innsbruck, Innsbruck, Austria; 2Department of Internal Medicine, Medical University of Innsbruck, Innsbruck, Austria
Background: Early graft dysfunction (EAD) complicates liver transplantation. In the light of changing donor characteristics and machine perfusion, the definition of EAD deserves reevaluation. The aim of this analysis was to discriminate between the single effect of each variable of EAD and to develop a model for individualized risk estimation for the clinical outcome in liver transplantation.
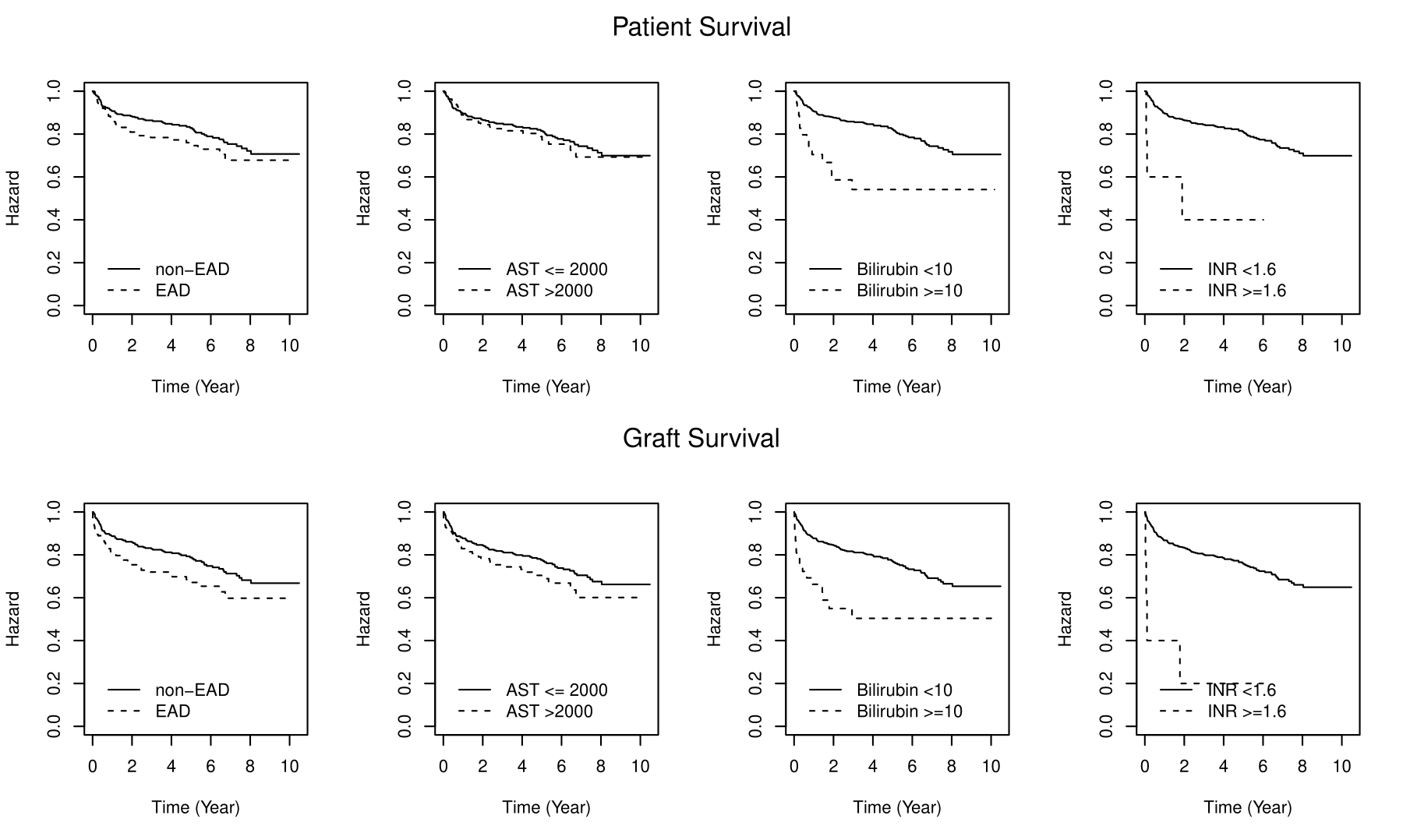
Material and Methods: We reviewed all primary LT performed between 2007 and 2018. Exclusion criteria were age < 18 years, living donor transplantation and split grafts. Primary endpoint was the discriminative value of each variable defining EAD, secondary endpoints were risk factors. EAD was recorded when at least one of the following criteria was present: (i) AST levels >2000 IU/L within the first seven days, (ii) bilirubin levels ≥10mg/dL or (iii) INR ≥1.6 on postoperative day 7. EAD parameter were assessed by developing a Cox proportional hazard model. Predictors for EAD were investigated using logistic regression analysis. Survival rates were compared using the Kaplan–Meier method.
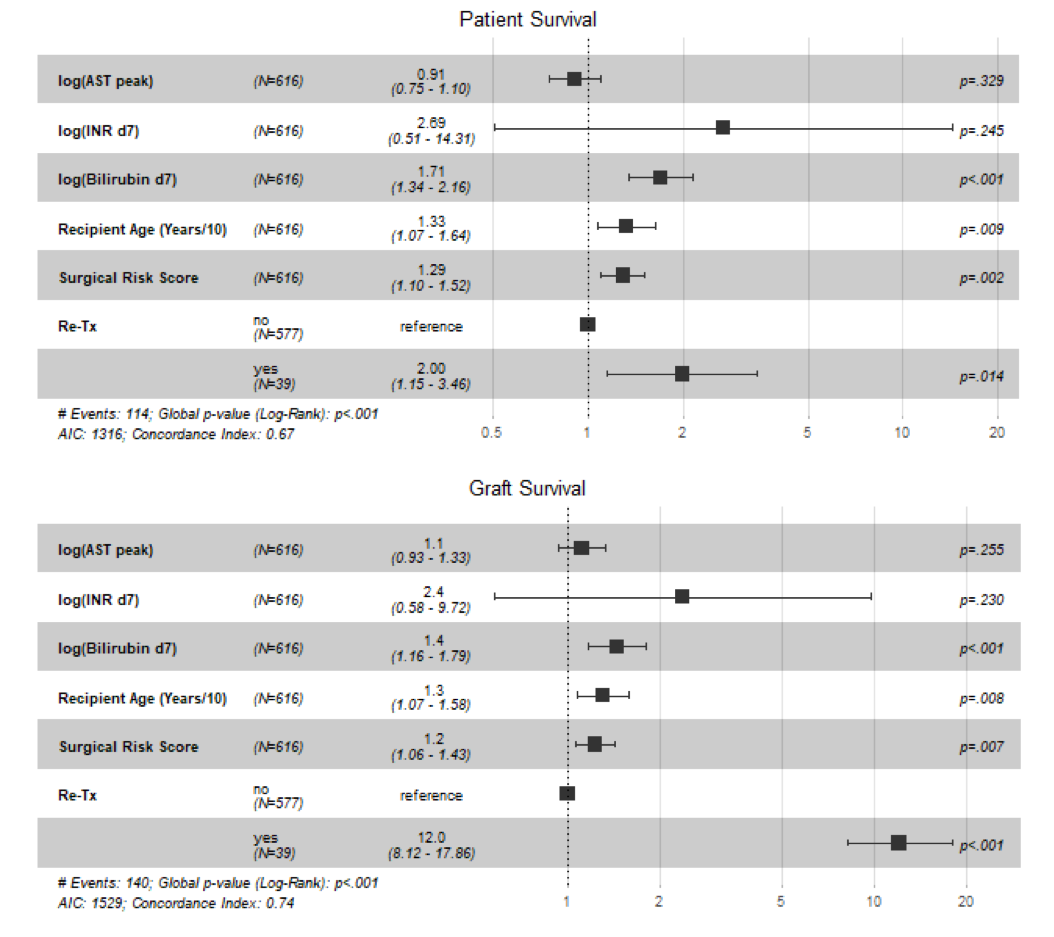
Results and Discussion: Six-hundred-sixteen LT were included. Of these, 30.7% developed EAD. Patient survival did not differ significantly between groups (P = .09; Log Rank-Test=2.87). Graft survival was significant higher in non-EAD patients (P =.008; Log Rank-Test=7.13). Isolated elevated AST (78%) and bilirubin (8%) were the most frequent variables in EAD recipients. The proportional hazard regression model showed strikingly diverse discriminative value of EAD parameter for prediction of mortality. While Bilirubin was the best predictor (W = 12.64, P < .001 for patient survival; W = 13.17, P < .001 for graft survival), AST did not serve to display a significant discrimination (W = 0.31, P = .580 for patient survival; W = 3.19, P = .074 for graft survival). Comparing the Hazard Ratio (HR) in Cox proportional hazard model, bilirubin and INR were selected as strong mortality predictors (Bilirubin HR = 1.71 [1.34, 2.16]; INR HR = 2.69 [0.51, 14.31]), while AST did not reach significant effect (HR = 0.91 [0.75, 1.10]) suggesting a categorized discrimination potential in EAD status. Similar results were achieved for graft loss estimation (Bilirubin HR = 1.44 [1.16, 1.79]; INR HR = 2.37 [0.58, 9.72]; AST HR = 1.11 [0.93, 1.33]. Child B Score, Child C Score, surgery duration, regional allocation, cold ischemia time, donor risk index and donor BMI > 25 were independent risk factors for EAD in this study.
AST levels as primary endpoint poorly reflect graft and patient survival, while bilirubin and INR have strong predictive capacity. This fits well with the idea that bile duct injury and deprivation of synthetic function rather than hepatocyte injury are key factors in liver transplantation.
Conclusion: New insights into the utility of EAD were presented. For an individualized risk estimation, we propose reconsideration of the EAD definition.
There are no comments yet...
