Technical refinement to prevent hepatic outflow disturbance in right lobe living donor liver transplantation: Simplified one-orifice venoplasty with artificial vascular graft
Joo Dong Kim1, Donglak Choi1, Eunkyoung Jwa1.
1Department of Surgery, Catholic University of Daegu College of Medicine, Daegu, Korea
Background: Middle hepatic vein (MHV) reconstruction is often essential to avoid hepatic congestion and serious graft dysfunction in living donor liver transplantation (LDLT). Homologous vein allograft has been traditionally regarded to be the most suitable conduit for MHV reconstruction but supply shortage is most serious problem. The aim of this report was to introduce evolution of our MHV reconstruction techniques and the excellent outcomes of simplified one-orifice venoplasty with artificial vascular graft.
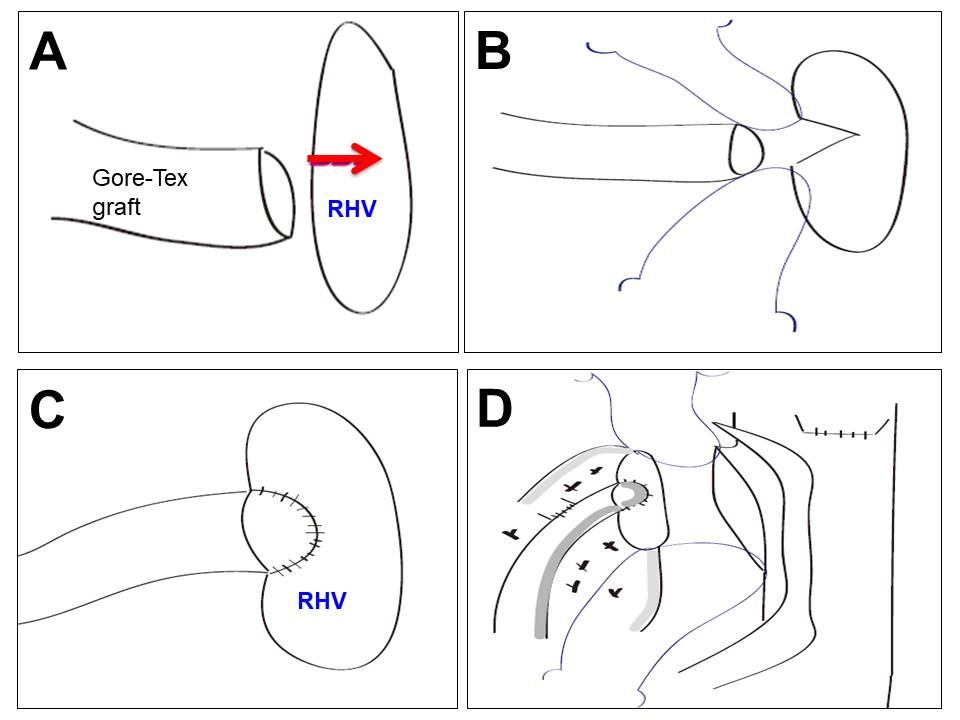
Materials and Methods : We compared clinical outcomes with three types of our MHV reconstruction techniques through retrospective review of 382 recipients who underwent LDLT using right lobe graft at our institution from January 2008 to December 2018; group I (n = 34) received separate outflow reconstruction, group II (n = 166) received one-orifice technique that create the wider single outflow with patchwork and group III (n = 182) received more simplified one-orifice technique that invaginate reconstructed MHV only with artificial graft (Gore-Tex graft) into right hepatic vein (RHV) without patch venoplasty.
Results : Patient demographics did not differ significantly between the three groups, but cold ischemic time and operation time in group II and III were significantly lower than those in group I (134.9 min versus 104.8 min versus 101.1 min, P = 0.000 and 546.9 min versus 398.4 min versus 331.3 min, P=0.000, respectively). No significant difference between the groups in postoperative infection was observed. The early patency rates of MHV in group II and III were higher than those in group I; 95.8%, 99.5% versus 85.3% on postoperative day 7 (p=0.000) and 91.0% and 96.2% versus 82.4% on postoperative day 14, respectively (p =0.010). Peak total bilirubin value (within one month after LDLT) in group I and II was significantly higher than that in group III (8.3mg/dL and 6.5mg/dL versus 4.9mg/dL, p=0.009). Especially, MHV or RHV stent insertion during the early post-transplant period only occured in one patient (0.5%) in group III during follow-up periods.
Conclusion: This technique is easy to perform without a learning curve or complex venoplasty using autologous vein or homologous vein graft. Furthermore, our new simplified one-orifice technique with artificial vascular grafts could be an effective method of overcoming technical difficulties and the outflow disturbance in right lobe LDLT without complex bench work to create large outflow and solve the problem related with supply shortage for homologous vessel allografts.
There are no comments yet...
