83% 10 year survival rate after liver transplantation in 200 cases at a small volume center in Korea
Yang Won Nah1, Chang Woo Nam1, Hyung Woo Park2, Hong Rae Cho1, Sang Jun Park1, Ho Jong Park1, Sun Eun Park3, In Young Huh4, Jeong Rak Lee3, Jae Chul Hwang5, Young Woo Seo5.
1Department of Surgery, Ulsan University Hospital, Ulsan, Korea; 2Department of Surgery, SM Christianity Hospital, Pohang, Korea; 3Department of Anesthesiology, Ulsan University Hospital, Ulsan, Korea; 4Department of Anesthesiology, Asan Medical Center, Seoul, Korea; 5Department of Radiology, Ulsan University Hospital, Ulsan, Korea
Introduction: Korea is one of the countries where liver transplantation (LT) operation is being performed most actively in the world. According to the most recent data, KONOS reported 11 year patient survival rate after LT as 71.6% and UNOS reported the 10 year graft survival rate as 66.4%. The authors investigated the short-term and long-term results of LT performed at a small volume center in Korea.
Materials and Methods: From March 2002 to March 2019, 200 cases of adult LT were performed at Ulsan University Hospital. For these cases, the indications, operative data, early and late mortalities and long-term survival rates were investigated.
Results: 114 cases were performed with graft from deceased donor, including 5 cases of split right graft. There were 3 cases of simultaneous liver-kidney transplantation. Among 86 living donor liver transplantation (LDLT), ABO incompatible LDLT was performed in 15 cases (17.5%). The most frequent indication was HBV, comprised of 115 cases (57.5%), of which 75 cases were complicated by HCC. Alcohol and HCV comprised 22.5% and 9%, respectively. There were 96 cases of HCC in total and 15 LT’s were performed as a salvage operation. During the operation, mean transfusion amounts were 10 pints of RBC, 15 pints of FFP and 7 pints of PC. 15.8% of the operation was performed without RBC transfusion. There was no intraoperative mortality. 3 cases of retransplantation were performed within 30 days after the primary operation and all were developed after ABO incompatible LT. 10 Cases of 90-days mortality happened. The causes were sepsis (4), graft versus host disease (3), fulminant viral (herpetic) hepatitis (1), primary nonfunction (1) and portal vein thrombosis (1). Late mortality (death after 90 days) developed in 14 cases. The causes were HCC recurrence (8), de novo cancer (2), graft dysfunction (2), HCV recurrence (1) and systemic aspergillosis (1). Long-term survival rates were 92.4%, 86.8% and 83.7% at 1 year, 5 years and 10 years after LT, respectively. There was no significant difference in survival according to the indications (HBV vs. alcohol vs. HCC, Figure).
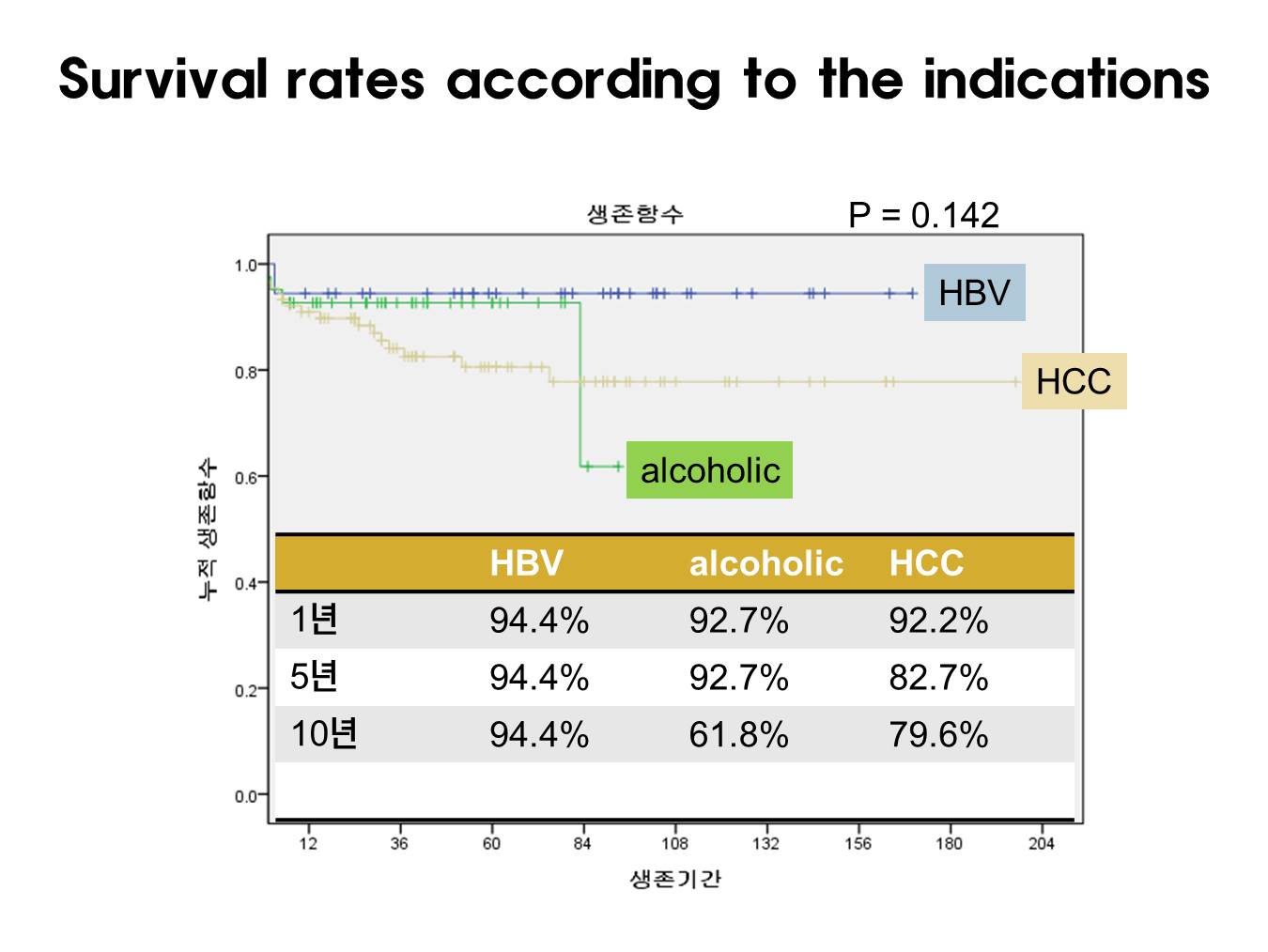
10 year survival rates for HCC was 79.6% and was 83.6% for within Milan group (n=69) and 68.6% for beyond Milan group (n=27, p=0.183).
Conclusion: In this era of widespread performance of liver transplantation in Korea, the short-term and long-term results were not influenced much from the volume of center. This may reflect through education of the transplant surgeons and other medical staves.
[1] KONOS. 장기등 이식 및 인체조직 기증 통계연보 2019.
[2] Kwong A, et al. OPTN/SRTR 2018 Annual Data Report: Liver. 2020. pp193-299.
There are no comments yet...
