ALBI grade at 30 days after transarterial radioembolization have poor prognosis after liver transplantation
Jorge Sanchez-Garcia1, Fidel Lopez-Verdugo1, Randie Riegler2, Maria Jepperson3, Andrew Gagnon1,4, Diane Alonso1, Shiro Fujita1,4, Manuel I. Rodriguez-Davalos1,5, Ramya Thota6, George Cannon7, Jake Krong8, Li Dong8, Sean Dow8, Richard Gilroy9, Mark Kringlen3, Ivan R. Zendejas-Ruiz1,4.
1Liver Transplant Service, Intermountain Medical Center, Murray, UT, United States; 2Imaging Research Service, Intermountain Medical Center, Murray, UT, United States; 3Interventional Radiology Service, Intermountain Medical Center, Murray, UT, United States; 4Canyon Surgical Associates, Intermountain Medical Center, Murray, UT, United States; 5Liver Transplant Service, Primary Children’s Hospital, Intermountain Healthcare, Salt Lake City, UT, United States; 6Oncology/Hematology Service, Intermountain Medical Center, Murray, UT, United States; 7Radiation Oncology Service, Intermountain Medical Center, Murray, UT, United States; 8Transplant Research Department, Intermountain Medical Center, Murray, UT, United States; 9Medical Director of Liver Transplant Service, Intermountain Medical Center, Murray, UT, United States
Introduction: Trans-arterial radioembolization (TARE) is a minimally invasive therapy that is effective for tumor downstaging and as bridge to liver transplantation (LT).The aim of this study is to identify the outcomes of TARE on patients with hepatocellular carcinoma (HCC).
Materials and methods: We retrospectively assessed all patients with HCC that underwent TARE between February 2008 and January 2020 at Intermountain Medical Center. Patients that underwent LT were included. Clinical and demographic characteristics were collected. ALBI score was calculated one month before (time zero) TARE, 30-, 90- and 180-days after TARE. Inferential analysis was performed with Chi-square test or a Fisher’s exact test depending on the variables. A Kaplan-Meier survival curve and log-rank test were performed to assess differences on survival rates.
Results and Discussion: 59 patients were included, 45 were males and 14 females. The median age was 59 (IQR 55-65). ALBI grade at time zero, 30-, 90- and 180-days after TARE are shown in Figure 1.
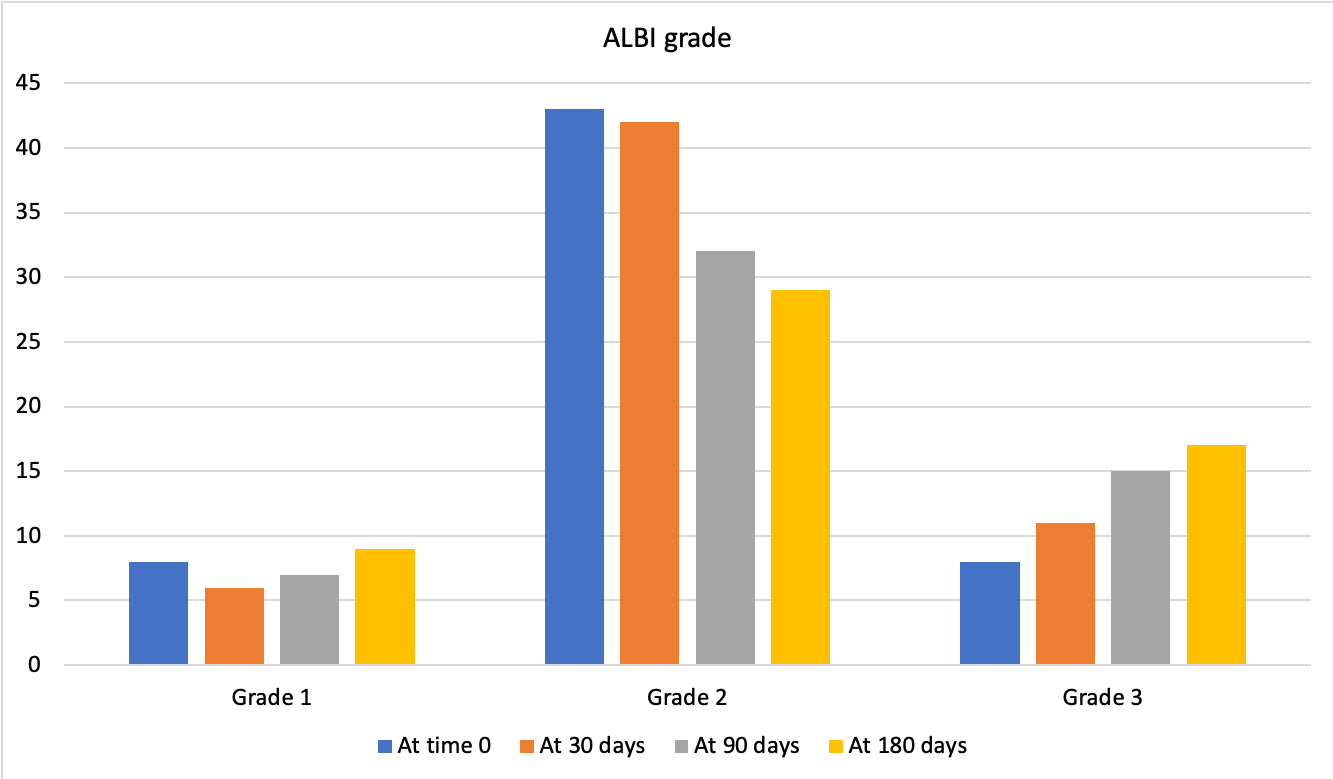
Eleven patients had ALBI grade 3 at 30-days (Group A) and 48 patients had ALBI grade 1-2 at 30-days (Group B). Group A was obese (7vs15, p=0.03), had single (10vs27, p=0.04) TARE lobectomy/segmentectomy (11vs32, p=0.02), higher lung-shunt fraction (7.4vs4.1p=0.007) and ALBI score was higher in all measurements(p<0.01). It is important to notice that 3 patients were downstage by ALBI grade at 30 days, 1 patient from 2 to 1, and 2 patients from 3 to 2. However, 9 patients were upstage by ALBI grade at the same time, 2 patients from 1 to 2, and 5 patients from 2 to 3, the latter subgroup had 100% of mortality while the other three subgroups didn’t have any mortality. It is important to notice that no statistically significant difference in recurrence was found between the groups. Kaplan-Meier survival curve showed that Group A had worse overall survival compared to Group B (p=0.01, Figure 2), when we did the same analysis with ALBI grade before TARE no statistically significant difference was found.
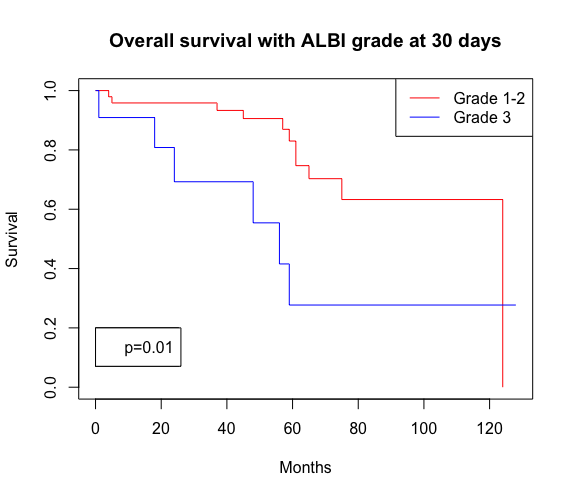
LT has better outcomes for HCC, despite this we are reporting that ALBI grade 3 at 30 days after TARE identified patients that decompensate with poor survival after LT. It should be pointed out that the patients that were ALBI grade upstage from 2 to 3 had a 100% of mortality after LT in the study period. Patients with obesity and higher lung-shunt fraction with TARE lobectomy/segmentectomy are some of the hypotheses to explain these discrepant outcomes but our small size sample is a limitation. Interestingly, further studies should be considered to compare patients downstage from 3 to 2 with the other subgroups.
Conclusion: TARE is a safe and effective neoadjuvant treatment for liver tumors. Interestingly, ALBI grade 3 at 30 days have poor prognosis compared to ALBI grade 1-2, this finding was not noted on ALBI grades before TARE and further studies are needed to assess this.
[1] Mohammadi H. Using the Albumin-Bilirubin (ALBI) grade as a prognostic marker for radioembolization of hepatocellular carcinoma. Journal of Gastrointestinal Oncology. 2018; 9(5): 840-846.
[2] Antkowiak M. Prognostic Role of Albumin, Bilirubin, and ALBI Scores: Analysis of 1000 Patients with Hepatocellular Carcinoma Undergoing Radioembolization. Cancers. 2019; 11: 879.
There are no comments yet...
