Liver transplantation in the United Arab Emirates: Initial two-year experience
Shiva Kumar1, Charles M. Miller2, Koji Hashimoto2, Cristiano Quintini2, Antonio Pinna1.
1Digestive Disease Institute, Cleveland Clinic Abu Dhabi, Abu Dhabi, United Arab Emirates; 2Transplant Center, Cleveland Clinic Foundation, Cleveland, OH, United States
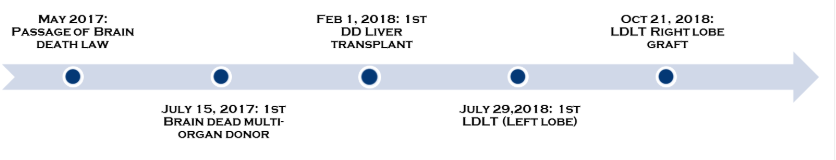
Background: Passage of the landmark brain death law in the United Arab Emirates (UAE) in May 2017 enabled the establishment of solid organ transplantation, including liver transplant (LT). The shortage of deceased donor (DD) organs mandated the development of living donor LT (LDLT) as well. We report our initial experience following the formal establishment of LT in the UAE.
Materials and Methods: The first DDLT and LDLT in the UAE were performed on Feb 1 and July 29, 2018 respectively.
Since inception, a total of 11 DDLTs and 12 LDLTs have been performed – 8 left-lobe and 4 right-lobe LDLTs. Five (22%) recipients were expatriates (four of whom underwent DDLT), while the remainder were UAE nationals. Primary indication for LT was NAFLD (48%). All four (17%) recipients with HCC had cirrhosis from NAFLD. Two recipients (9%) each underwent LT for PSC, Wilson’s disease, HBV and AIH. Two emergent LTs were performed - one for fulminant Wilson’s disease (left lobe LDLT), and the other for early graft dysfunction following LDLT. Mean graft to recipient weight ratio (GRWR) for LDLTs was 0.92 (range: 0.64 – 1.30). GRWR for left and right lobe grafts were 0.83 and 1.1 respectively. All but one of the left lobe recipients underwent splenectomy. All recipients underwent duct to duct biliary reconstruction.
Results: All living donors recovered uneventfully with a median duration of hospitalization of 6.5 days (6 and 8 days respectively for left and right lobe donors).
Two recipients underwent unplanned re-operation within 30 days of LT. Four (17%) recipients developed acute cellular rejection. All episodes were mild-moderate and responded to either escalation of immunotherapy or pulse steroids, with the exception of one severe episode due to non-compliance. CMV viremia was noted in 11, with invasive disease (retinitis) occurring only in one recipient. Four DDLT and 6 LDLT recipients developed biliary strictures, all of which were anastomotic in nature and responded promptly to endoscopic therapy, with the exception of four post-LDLT strictures that required more than 3 ERCPs.
14 recipients have completed at least a year of follow up, with one-year actual graft and patient survival of 100% and 100% respectively. The overall patient and graft survival for the 22 patients and 23 grafts were 100% and 96% respectively. The solitary graft loss occurred due to portal vein steal syndrome via coronary vein shunt following left lobe LDLT causing graft dysfunction, necessitating emergent DDLT.
Conclusions: We report the successful establishment of LT from living and deceased donors in the UAE and our results after the first two years. Ongoing efforts to overcome shortage of deceased donor organs include creation of a national digital donor registry, regional organ sharing agreements for critically ill patients and establishment of donation after circulatory death. These initiatives will enable us to build on our early success and meet the anticipated increase in demand for LT related to the growing burden of NAFLD in the region.
There are no comments yet...
