
Living donor liver transplantation and intention to use segmental grafts increases transplant rates and decreases waiting time at a single institution
Fidel Lopez-Verdugo1,2, Jorge Sanchez-Garcia1,2, Shani Baraki1, Zachary J. Kastenberg3, Jesus E. Sanchez-Garavito1, Andrew I. Gagnon1,2, George Rofaiel1,4, Ivan R. Zendejas-Ruiz1,2, Jeffrey Campsen1,4, Diane Alonso1,2, Robin D. Kim1,4, Shiro Fujita1,2, Manuel I. Rodriguez-Davalos1,2.
1Liver Transplant Unit, Intermountain Primary Children's Hospital, Salt Lake City, UT, United States; 2Transplant Services, Intermountain Medical Center, Salt Lake City, UT, United States; 3Division of Pediatric Surgery, University of Utah School of Medicine, Salt Lake City, UT, United States; 4Division of Transplantation and Advanced Hepatobiliary Surgery, University of Utah School of Medicine, Salt Lake City, UT, United States
Introduction: Evidence shows comparable results between segmental (SG) and whole liver grafts, including better outcomes for living donor liver transplants (LDLT). In July 2017, our LDLT program was reestablished and a policy to increase the use of SG was implemented at our institution.
The aim was to compare wait list activity and outcomes between two time periods after implementation of a policy to increase the use of segmental grafts and reestablishment of a LDLT program.
Materials and Methods: Single center, retrospective study. Pediatric patients on the liver waiting list between January 2015 and December 2019 were screened. Simultaneous liver-kidney and re-transplants were excluded.
Patients were classified as receiving a LT before (Period 1) or after (Period 2) policy changes (Fig 1).
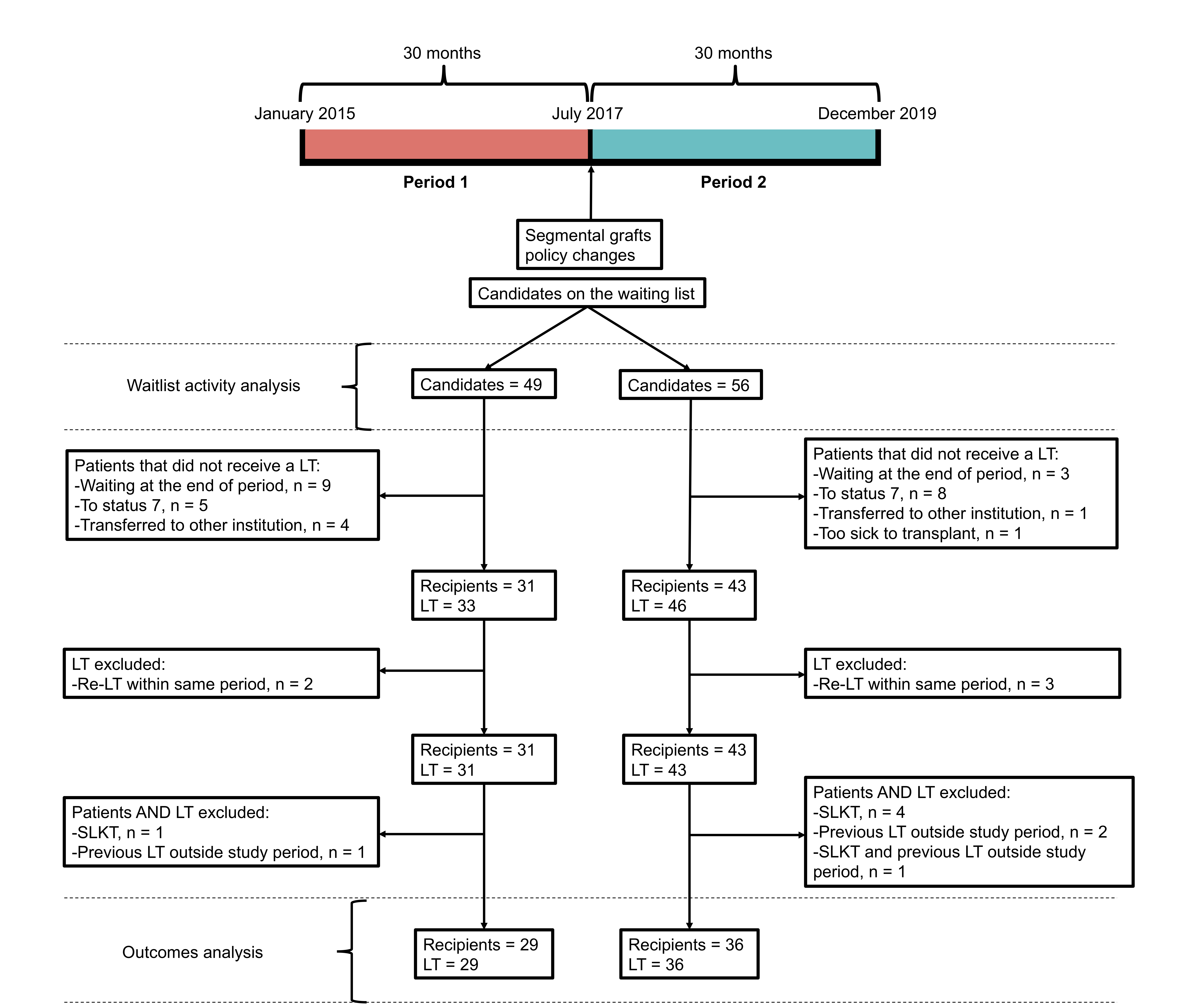
For waitlist activity analysis, person-years and transplant rates per 100 person-years on the waiting list were calculated. For outcomes analysis, patients who received a first LT were included. Primary endpoints were transplant rates per 100 person-years and time-to-transplant. Secondary outcomes included complication rates, and patient and graft survival.
Results and Discussion: 79 LTs were performed on 74 pediatric patients. 65 first LT performed on 65 patients were included. 29 LT were performed during Period 1 and 36 during Period 2. 31 (47.7%) were female with a median age of 38 months (Table 1).
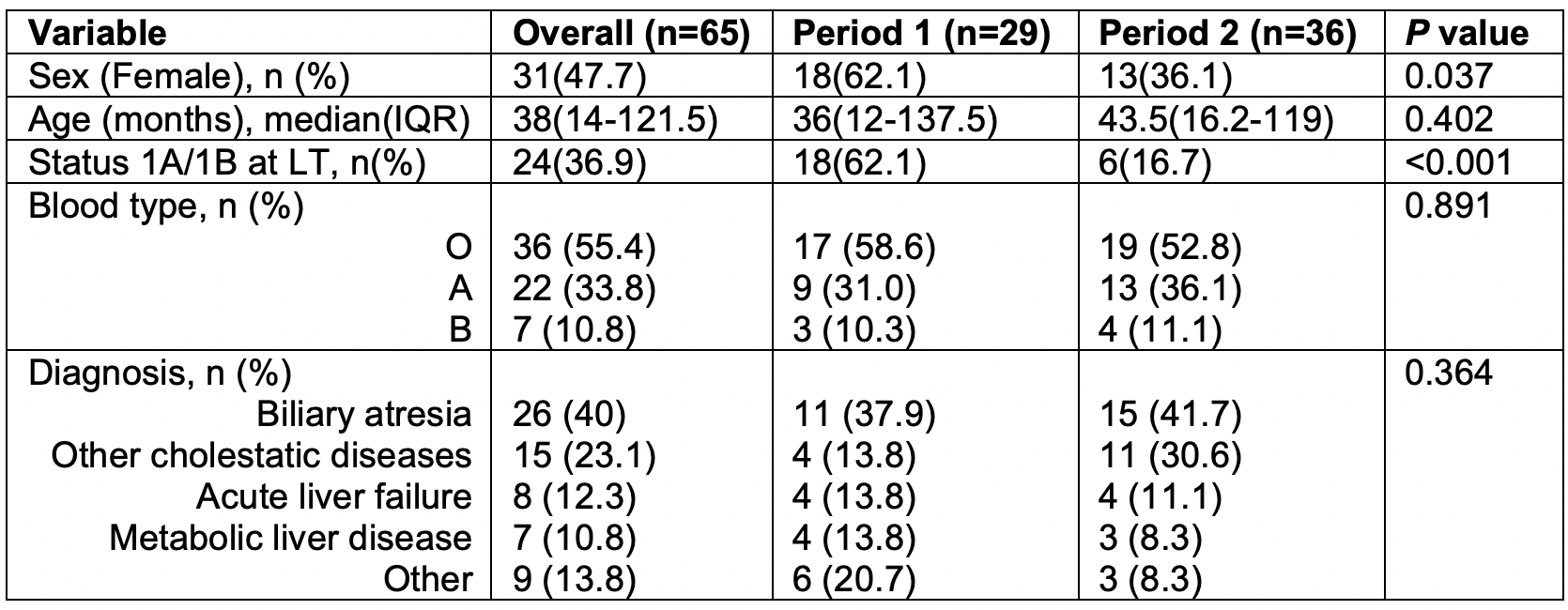
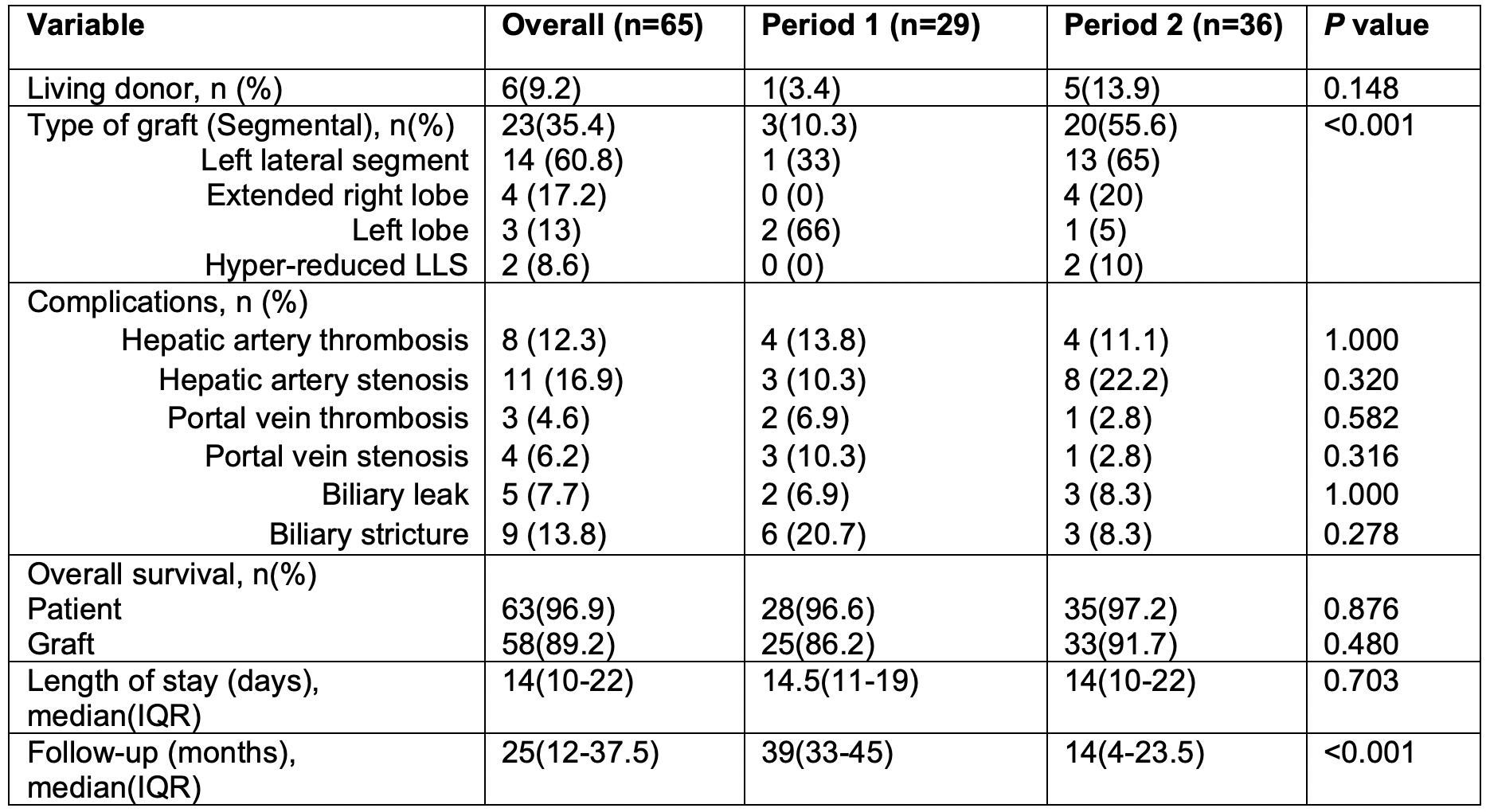
LDLTs increased from 3.4% to 13.9% in Period 2 (p = 0.148). 55% of LT in Period 2 were segmental grafts, compared to 10.3% in Period 1 (p < 0.001). The most common grafts used were left lateral segments (60.8%) (Table 2).
49 and 56 pediatric candidates on the waiting list accounted for 38.78 and 24.48 person-years during Period 1 and Period 2, respectively. Transplant rates per 100 person-years on the waiting list increased from 56.0585.09114.12 during Period 1 to 133.58187.87242.16 in Period 2 (Rate ratio: 1.412.203.45; p < 0.001). Median time to receive a LT decreased from 153229512 days in Period 1 to 5275143 days during Period 2 (Fig 2).
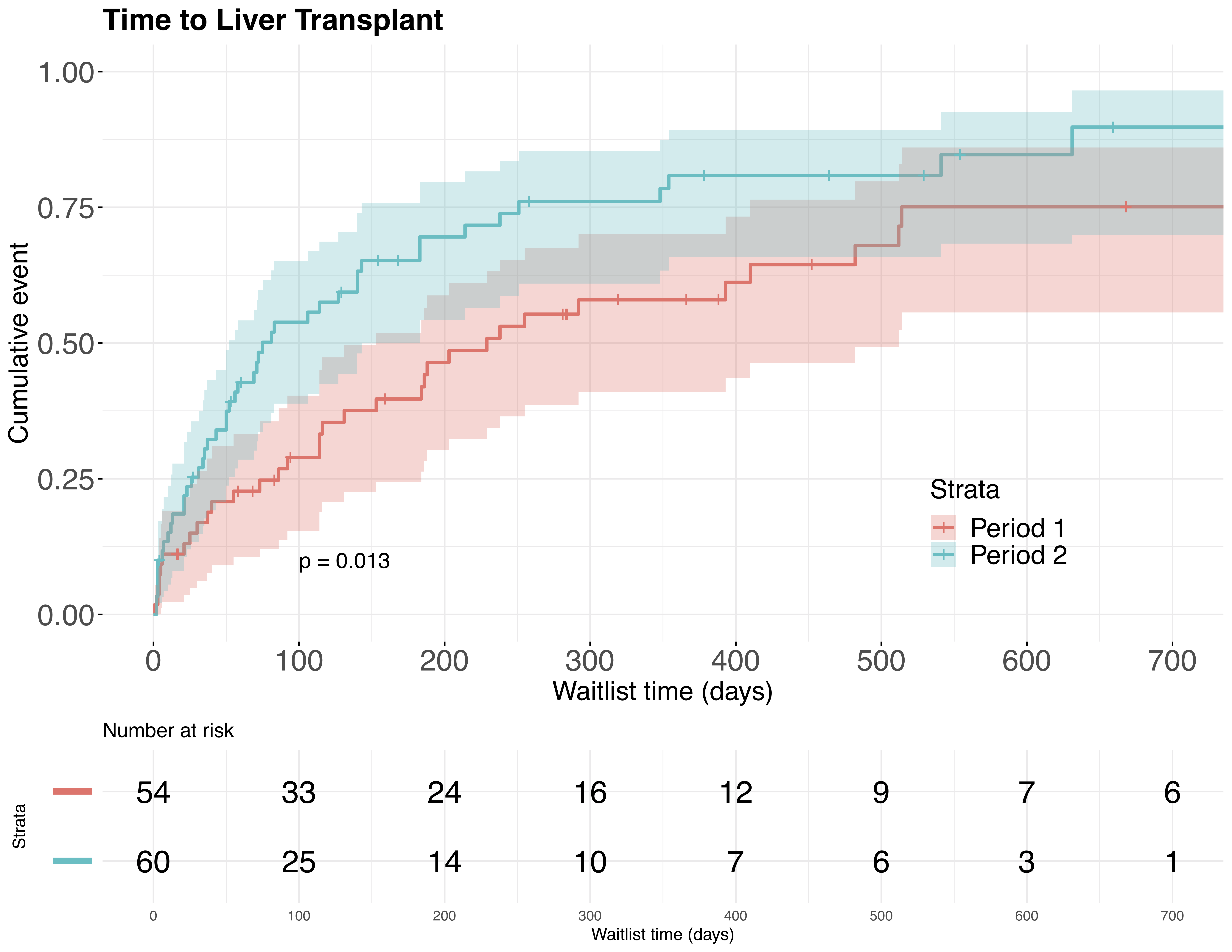
Cox regression model yielded a hazard ratio of 1.121.762.76, meaning 76% increased odds of receiving a LT earlier after implementation of the policy (p= 0.013).
There were no statistically significant differences in vascular and biliary complication rates between both groups. There was no statistically significant difference in one-year and overall patient and graft survival between both periods (Table 2).
Conclusion: A policy to increase the use of SG significantly increased transplant rates and decreased waiting times to get a LT and can be successfully implemented at single pediatric institutions. Implementation of this policy can be done while maintaining patient and graft survival. Regional collaboration between centers performing pediatric and adult LT is key to the success of SLT.
[1] Moussaoui D, Toso C, Nowacka A, et al. Early complications after liver transplantation in children and adults: Are split grafts equal to each other and equal to whole livers? Pediatr Transplant. 2017;21(4). doi:10.1111/petr.12908
[2] Battula NR, Platto M, Anbarasan R, et al. Intention to Split Policy: A Successful Strategy in a Combined Pediatric and Adult Liver Transplant Center. Ann Surg. 2017;265(5):1009-1015. doi:10.1097/SLA.0000000000001816
[3] Mogul DB, Luo X, Bowring MG, et al. Fifteen-Year Trends in Pediatric Liver Transplants: Split, Whole Deceased, and Living Donor Grafts. J Pediatr. 2018;196:148-153.e2. doi:10.1016/j.jpeds.2017.11.015
There are no comments yet...
