Pregnancy outcomes in 36 lung transplant recipients
Theresa A. Daly1, Lisa Coscia1, Howard M. Nathan2, Richard D. Hasz2, Serban Constantinescu1,3, Michael J. Moritz1,4,5.
1Transplant Pregnancy Registry International, Gift of Life Institute, Philadelphia, PA, United States; 2Gift of Life Donor Program, Philadelphia, PA, United States; 3Medicine, Lewis Katz School of Medicine at Temple University, Philadelphia, PA, United States; 4Surgery, Lehigh Valley Health Network, Allentown, PA, United States; 5Surgery, Morsani College of Medicine, Tampa, FL, United States
The purpose of this study is to describe 49 pregnancies in 36 lung transplant recipients reporting to the Transplant Pregnancy Registry International (TPR) from 1992-2019. Data were collected via questionnaires, telephone interviews, and medical records review. Data are listed in the table below. Cystic fibrosis was the reason for transplant in 20 of the women.
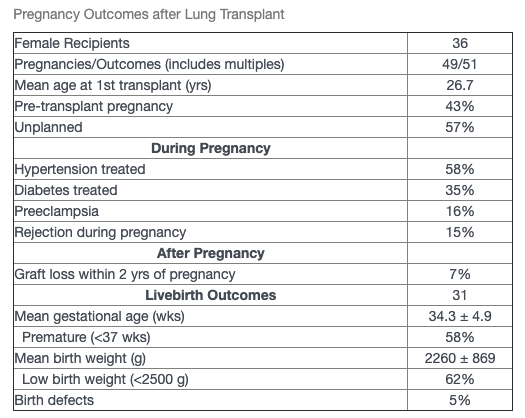
The majority of recipients were on calcineurin inhibitor therapy for immunosuppression; 21% on cyclosporine and 79% on tacrolimus; 14% of pregnancies were exposed to a mycophenolic acid product (MPA) during the first trimester. There were a total of 51 pregnancy outcomes (including multiples) resulting in 31 live births (61%), miscarriages (28%), terminations (10%), stillbirths (0) and ectopic pregnancies (2%). There were 6 first trimester exposures to MPA resulting in 3 miscarriages, 2 live births (no birth defects) and 1 neonatal death due to prematurity (26 wks) also umbilical cord anomally. Livebirth outcomes are listed in the table. There were 8 infants who were breastfed. The TPR has been following the offspring long-term: mean age of the children 8.6 ± 7.8 yrs. With a mean maternal follow-up of 9.3 ± 7.6 yrs, 9 recipients have died, 2 reported reduced function,1 with return of native function, 1 unknown, and 23 reported adequate transplant function.
Conclusions: Successful pregnancy is possible after lung transplantation, though caution is advised as these are extremely high-risk pregnancies with high incidences of graft rejection, prematurity, low birthweight infants. Close surveillance of these recipients is warranted due to the negative impact of rejection during pregnancy on graft and long-term maternal survival. All centers worldwide are encouraged to have their recipients report all pregnancies to the TPR.
[1] Transplant Pregnancy Registry International (TPR) 2018 Annual Report, Gift of Life Institute, Philadelphia, PA 2019.
[2] Shaner J, Coscia LA, Constantinescu S, et al. Pregnancy after Lung Transplantation. Progress in Transplant 2012;22(2):134.
There are no comments yet...
