Emerging roles of left ventricular assist device therapy as bridge to transplant in an Asian city with scarce heart transplant donor
Ka Lam Wong1, Cally Ho2, Timmy WK Au2, SL Lam2, KY Cheng1, KL Au1, YM Chow1, Katherine Fan1.
1Cardiac Medical Unit, Grantham Hospital, Hong Kong, Hong Kong; 2Department of Cardiothoracic Surgery, Queen Mary Hospital, Hong Kong, Hong Kong
Introduction: Limited organ availability remained a major hurdle for heart transplant in Hong Kong (HK). In 2019, there were only 8 heart transplantations in a 7.5 million populations. This had negative impact on the time and mortality on transplant waiting list. Left ventricular assist device (LVAD) has been used as a bridge to transplantation. This study aimed to assess the impact of implementation of LVAD therapy on heart transplant service.
Materials and Methods: All patients who had been put on heart transplant waiting list since the start of our heart transplant program in HK in 1992 until December 2019 were included. Our LVAD program started in 2010 and patients were stratified into pre-LVAD era 1992-2009 and post-LVAD era 2010-2019. Survival were analyzed by Kaplan Meier analysis and compared by Log-rank test. Survival free from the need of LVAD were also analyzed and compared among groups.
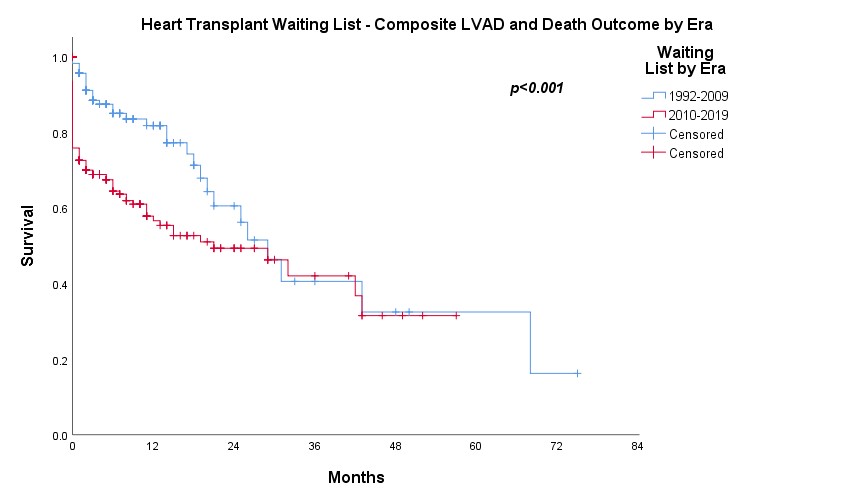
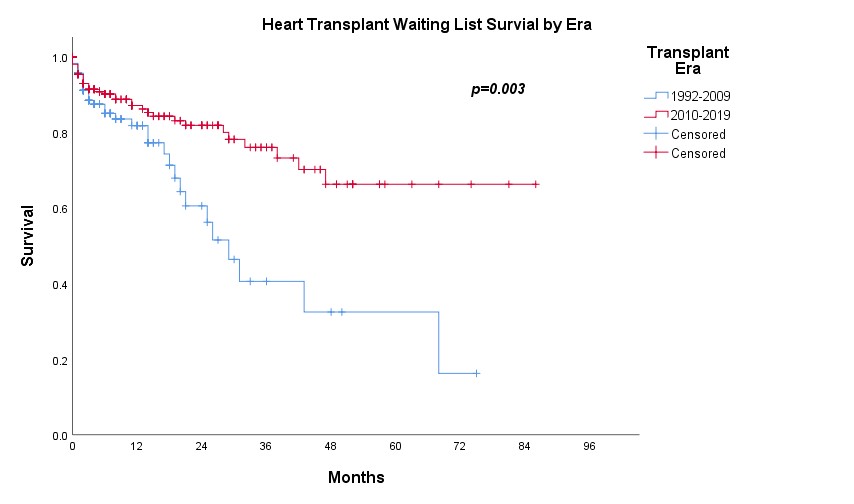
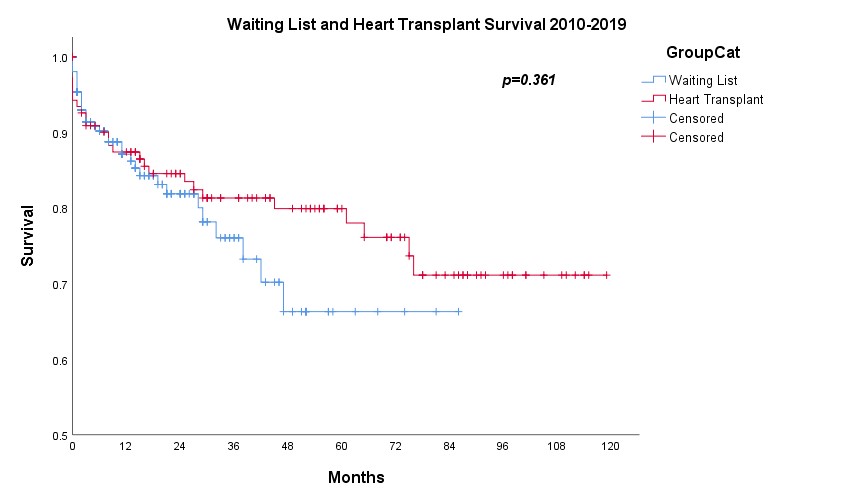
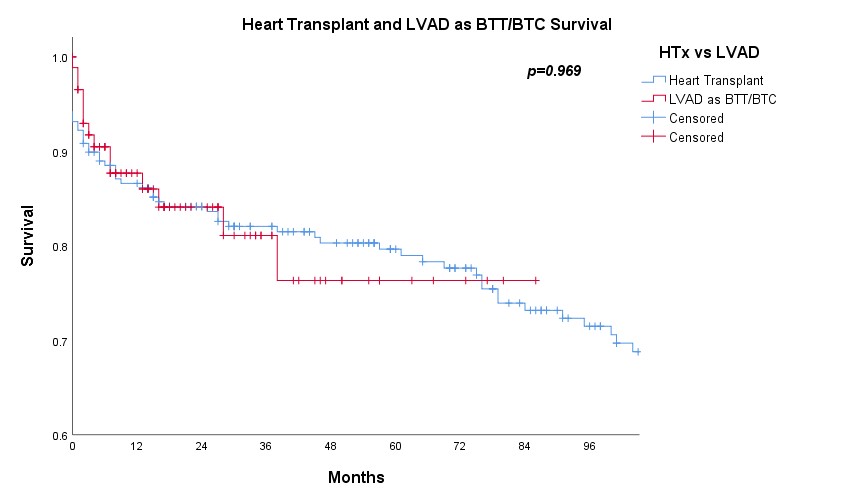
Results: A total of 432 patients were included for analysis, among which 219 had undergone heart transplantation. There were 88 patients received LVAD as bridge to transplantation (BTT) or bridge to candidacy (BTC) and 25 had subsequent heart transplantation. In the pre-LVAD era, the 1-, 2- and 3-year survival on waiting list were 81.8%, 60.6% and 40.6% respectively (n=175) while 1-, 2- and 3-year survival free from LVAD were 56.6%, 49.4% and 42.1% respectively in the post-LVAD era (n=257) (p<0.001) (Figure 1). However, the actuarial survival on waiting list in the post-LVAD era was significantly improved with 1-, 2- and 3-year survival 87.1%, 81.9% and 76.1% (p=0.003) (Figure 2). There was no significant difference on survival on waiting list and after heart transplantation (p=0.361) (Figure 3) as well as on survival after heart transplantation and after LVAD as BTT/BTC (p=0.969) (Figure 4) in the post-LVAD era.
Discussion: In pre-LVAD era, annual mortality on waiting list was about 20%. In the post-LVAD era, although there were more patients with more sick profile being put on waiting list as reflected by lower survival free from the need of LVAD, the actuarial survival on waiting list was significantly better likely contributed by good LVAD outcome. However, the increasing number of patients on heart transplant waiting list was not matched with the scarce organ availability and thus resulting in progressive longer waiting list. In fact, our local data suggested the survival post LVAD as BTT/BTC appeared to be comparable to heart transplant survival and thus it seemed reasonable to put patients stable on LVAD a lower priority on transplant waiting list.
Conclusion: Waiting list survival improved in the post-LVAD era especially among LVAD recipients. Thus given the scarce organ availability, it might be reasonable triage patients stable on LVAD therapy a lower priority on transplant waiting list or even as semi-"destination therapy".