Pediatric primary deceased-donor-kidney transplant-recipients outcomes by immunosuppression induction received in the United States
Samy Riad1, Scott Jackson 2, Srinath Chinnakotla 3, Priya Verghese 4.
1Medicine , University of Minnesota , Minneapolis, MN, United States; 2Complex Care Analytics , M-Health-Fairview , Minneapolis, MN, United States; 3Surgery , University of Minnesota , Minneapolis, MN, United States; 4Pediatrics, Northwestern University Feinberg School of Medicine, Chicago , IL, United States
Objective: We studied the influence of induction type on patient and kidney graft survival in pediatric recipients of deceased-donor kidneys.
Material and Methods: We analyzed the SRTR standard analysis file to evaluate all primary pediatric deceased donor kidney transplants through December 2017.
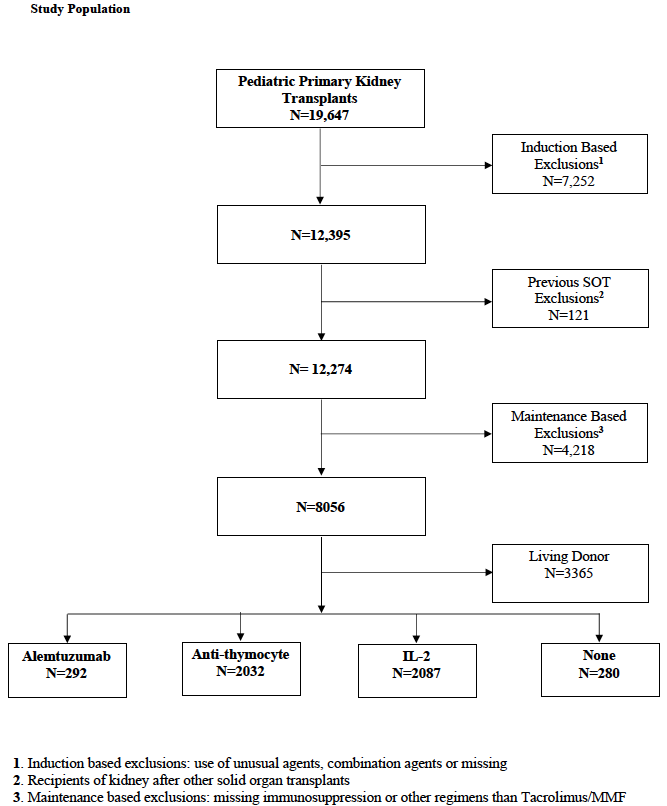
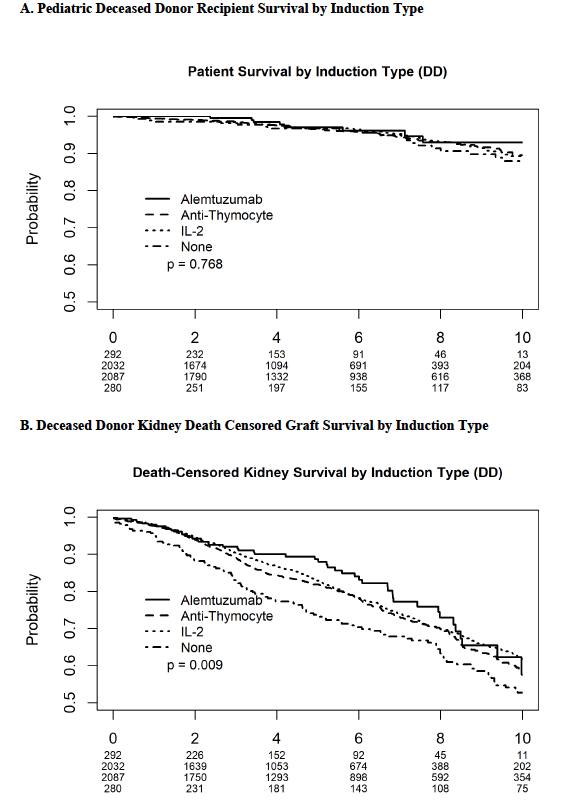
We included only recipients who were maintained on tacrolimus and mycophenolate. Recipients were grouped by induction type; into four groups: Alemtuzumab n= 292, Anti-thymocyte n= 2032, Interleukin-2 (IL-2) n=2087, and No-induction (steroid only) n= 280. Kaplan-Meier curves were generated for recipient and death censored graft survival.
Recipient and allograft survival and their predictors were examined using Cox proportional hazards models. Models were adjusted for age, sex, ethnicity, HLA-antigen mismatches, PRA, transplant year, steroid maintenance, preemptive transplantation and payor type, with transplant center included as a random effect.
Results: Rejection rates did not significantly differ between groups. In the multivariate models, the induction type did not influence patient survival. Death-censored graft survival (DCGS) was significantly different between induction types and IL-2 was associated with a 24.7% [HR 0.753, P= 0.015] improved graft survival over no induction in the multivariate model. Black race, public payor and female sex were poor predictors of the overall recipient’s survival.

Conclusion: In this large cohort of pediatric primary deceased-donor kidney recipients, induction use did not influence pediatric patients’ survival. Graft survival was significantly different among different types of induction, with no induction having the worst graft survival. In the multivariate analysis, only IL-2 was associated with a graft survival benefit. Racial, payor type- and sex-based outcome-disparities were significant outcome predictors in this group.
M-Health Fairview . University of Minnesota.
Manuela Marchetti
2021-03-29 23:31
Great Presetation