Pediatric primary live-donor-kidney transplant-recipients outcomes by immunosuppression induction received in the United States
Samy Riad1, Scott Jackson 2, Srinath Chinnakotla 3, Priya Verghese 4.
1Medicine, University of Minnesota, Minneapolis, MN, United States; 2Complex Care Analytics, M-Health-Fairview, Minneapolis, MN, United States; 3Surgery, University of Minnesota, Minneapolis, MN, United States; 4Pediatrics, Northwestern University Feinberg School of Medicine, Chicago, IL, United States
Objective: We studied the influence of induction type on patient and kidney graft survival in pediatric recipients of live-donor kidneys.
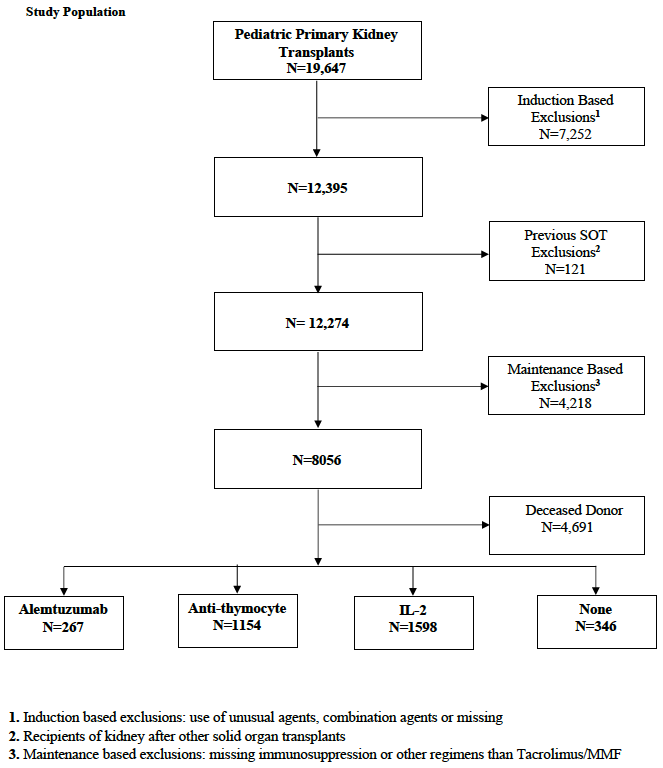
Material and Methods: We analyzed the SRTR standard analysis file to evaluate all primary pediatric deceased donor kidney transplants through December 2017. We included only recipients who were maintained on tacrolimus and mycophenolate. Recipients were grouped by induction type; into four groups: Alemtuzumab n= 267, Anti-thymocyte n= 1154, Interleukin-2 (IL-2) n=1598, and No-induction (steroid only) n= 346.
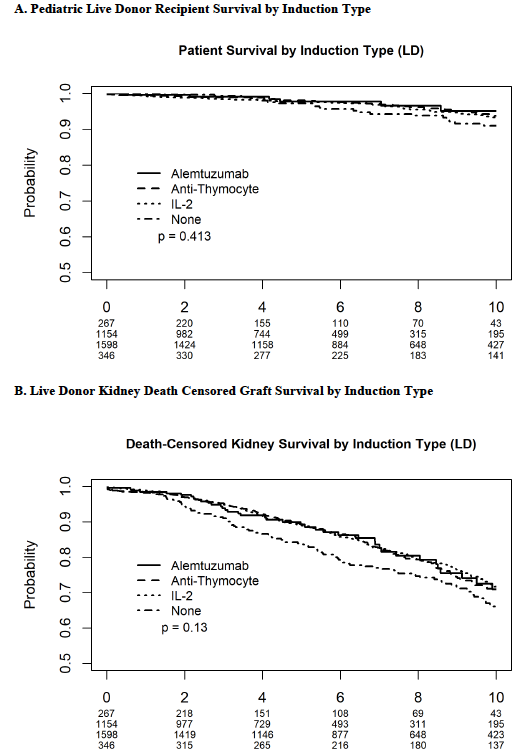
Kaplan-Meier curves were generated for recipient and death censored graft survival.
Recipient and allograft survival and their predictors were examined using Cox proportional hazards models. Models were adjusted for age, sex, ethnicity, HLA-antigen mismatches, PRA, transplant year, steroid maintenance, preemptive transplantation and payor type, with transplant center included as a random effect.
Results: Rejection rates did not significantly differ between groups. In the multivariate models, the induction type did not influence patient survival or death censored graft survival. Contrary to our findings in the recipients of deceased-donor kidney transplants, Black race, public payor and female sex were not predictors of the overall recipient’s survival. Preemptive transplantation was associated with improved recipient [HR 0.58, p 0.013]and graft survival [HR 0.72, p 0.001]. The higher the degree of HLA mismatches, the worse the patient and graft survival.
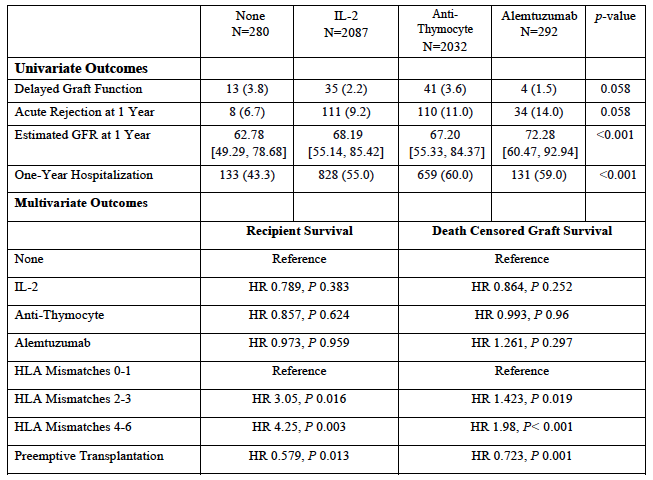
Conclusion: In this large cohort of pediatric primary live-donor kidney recipients, induction use did not influence patient or graft survival. Preemptive transplantation and close HLA matching portended strong patient and graft survival benefits in pediatric recipients of live-donor kidneys.
M-Health Fairview. University of Minnesota.
There are no comments yet...