
Survival Benefit of Pig-to-Baboon Liver Xenotransplantation Utilizing Genetically Modified Swine
Taylor M. Coe1, Danielle Detelich1, Charles G. Rickert1, Nikolaos Serifis1, Rudy Matheson1, Ivy Rosales1, Heidi Yeh1, Wenning Qin2, Yinan Kan2, Jacob Layer2, Michele Youd2, William Westlin2, Luhan Yang2, Shoko Kimura1, James F. Markmann1.
1Surgery, Massachusetts General Hospital, Boston, MA, United States; 2eGenesis, Cambridge, MA, United States
Introduction: Pig-to-baboon liver xenotransplantation (LXT) continues with significant hurdles, including thrombocytopenia, coagulation dysregulation and rejection. The longest reported pig-to-baboon LXT recipients survived 25 and 29 days utilizing GTKO pigs with continuous administration of human clotting factors. Herein, we report the results from seven pig-to-baboon LXTs with novel genetically modified swine in an attempt to mitigate anti-xeno immunity and physiologic incompatibilities.
Materials & Methods: 7 pig-to-baboon LXTs were performed from 3 lines of triple knock out (TKO), CMV-negative genetically modified pigs (Pig 2.05, 2.09, 2.10) that varied in their expression of human transgenes for complement regulatory proteins and genes targeting cellular immunity and inflammation. Immunosuppression consisted of anti-rhesus anti-thymocyte globulin (ATG), anti-CD20 antibody, methylprednisone taper, mycophenolate mofetil and anti-CD154 antibody. All recipients received a continuous infusion of human Prothrombin Complex Concentrate. Graft function was assessed with standard laboratory analyses including CBC, liver function tests (LFTs), coagulation factor levels and graft histopathology.
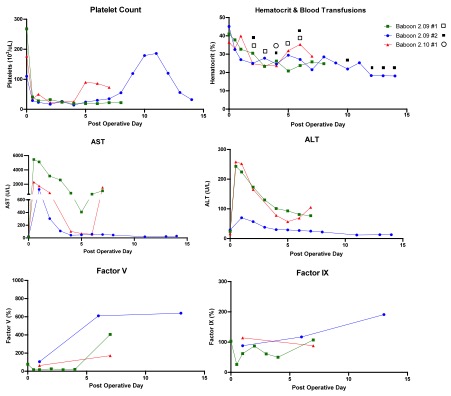
Results: Two Pig 2.05, one Pig 2.09 and one Pig 2.10 LTX recipients experienced pronounced reperfusion injury with coagulopathy, hemorrhage, and lung injury and were euthanized six hours post operatively. Of the three surviving animals, LFTs normalized between POD4-7. Each baboon manifested thrombocytopenia, with spontaneous recovery beginning on POD4 and 8. Consumption of coagulation factors occurred immediately after LXT, with subsequent production consistent with normal pig levels. Baboon 2.09#1 was euthanized on POD8 due to respiratory failure secondary to fluid overload; necropsy liver pathology showed focal ischemia without rejection and negative C4d. Baboon 2.09#2 had a normal protocol biopsy on POD8 but developed hemoptysis, necessitating euthanasia on POD14. Liver histology showed diffuse sinusoidal neutrophilic infiltrate, which may suggest an infectious process or xenograft rejection, however C4d was negative. Baboon 2.10#1 recovered uneventfully and required only one blood transfusion. On POD7, a rise in bilirubin and LFTs prompted exploration, where a bile leak with subsequent hepatic artery thrombosis was identified, requiring euthanasia. Liver histology confirmed focal subcapsular necrosis with negative C4d and no evidence of rejection, consistent with hepatic artery thrombosis.
Discussion: Our initial results of LXT with TKO pigs with modifications targeting complement, immune and inflammation regulation demonstrate that antibody-mediated rejection-free survival is attainable without splenectomy or use of cobra venom factor.
Conclusion: Life sustaining liver xenotransplantation is achievable with a clinically relevant immunosuppressive regimen and supplementation of clotting factors.
[1] Shah JA, Patel MS, Elias N, et al. Prolonged Survival Following Pig-to-Primate Liver Xenotransplantation Utilizing Exogenous Coagulation Factors and Costimulation Blockade. Am J Transplant 2017; 17(8):2178-2185.
[2] Patel MS, Louras N, Vagefi PA. Liver xenotransplantation. Curr Opin Organ Transplant 2017; 22(6):535-540.
There are no comments yet...