
Surgical management of intestinal failure: Initial experiences from an intestinal failure, rehabilitation and transplant unit in Iran
Hamed Nikoupour1, Peyman Arasteh1, Alireza Shamsaeefar1, Hesameddin Eghlimi1, Ali Mohammad Moradi1, Mohammad Yasin Karami1, Mojtaba Shafiekhani1, Gabriel E Gondolesi2, Saman Nikeghbalian1.
1Shiraz Transplant Center, Abu-Ali Sina Hospital, Shiraz University of Medical Sciences, Shiraz, Iran (Islamic Republic of); 2Unidad de Insuficiencia, Rehabilitacion y Trasplante Intestinal, Hospital Universitario Fundación Favaloro, Buenos Aires, Argentina
Background: Intestinal failure (IF) is a life-threatening medical condition. The Management of intestinal failure in low- and middle-income countries without home parenteral nutrition (HPN) remains unclear. We recently established an intestinal rehabilitation unit and aimed to provide our experiences on the current management and outcomes of IF in Iran.
Methods: In this cross-sectional case series, data were collected from an established data base on IF in the Shiraz Transplant Center in Abu Ali Sina Hospital, affiliated to Shiraz University of Medical Sciences, Iran during January 2018 and October 2018.
Results: Overall, 30 patients with a mean age of 44.13±10.32 years, which included 25 males, were included. Short bowel syndrome (SBS) (60%) and enterocutaneous fistulaes (27%), as complication of previous surgeries, were the main causes of IF. Most common type of IF was type 3 (67 %). Mesenteric Ischemia was the leading mechanism of IF (47%). Fifteen patients (50%) received autologous gastrointestinal reconstruction surgery, and 2 (7%) patients had serial transverse enteroplasty (STEP). At the end of follow-up, 15 patients recovered from IF (50%). The overall survival rate was 83.3%.
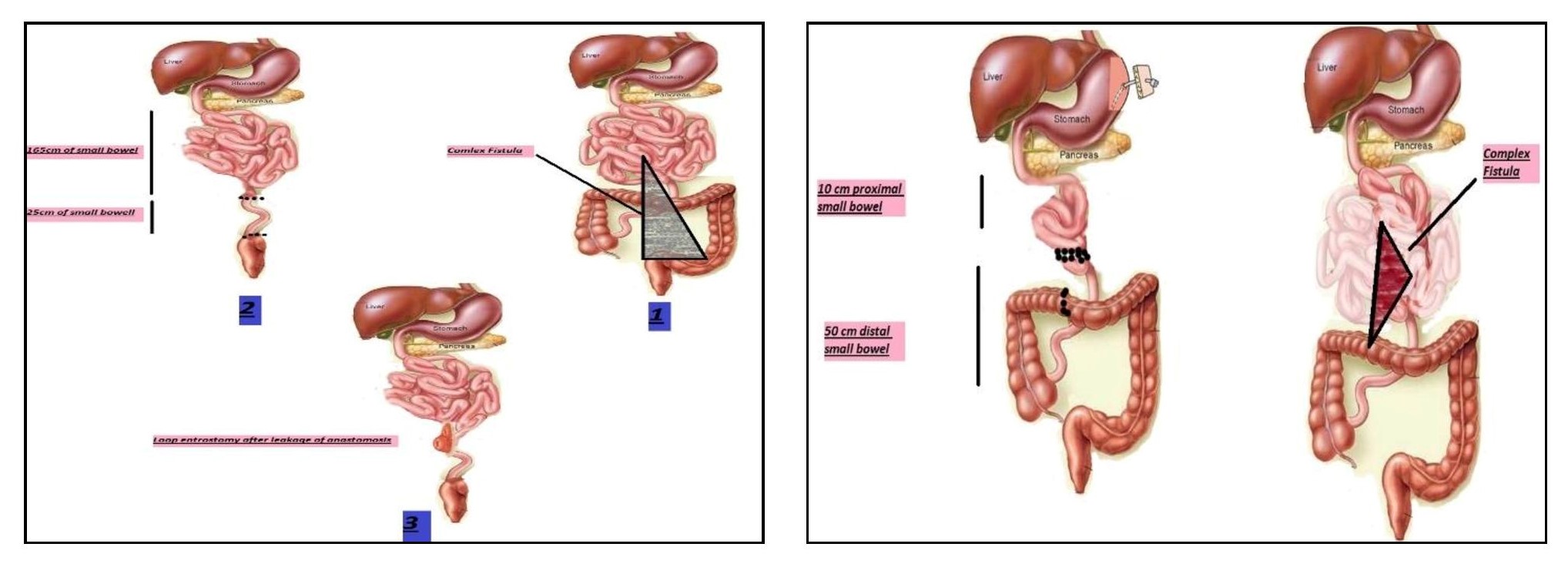

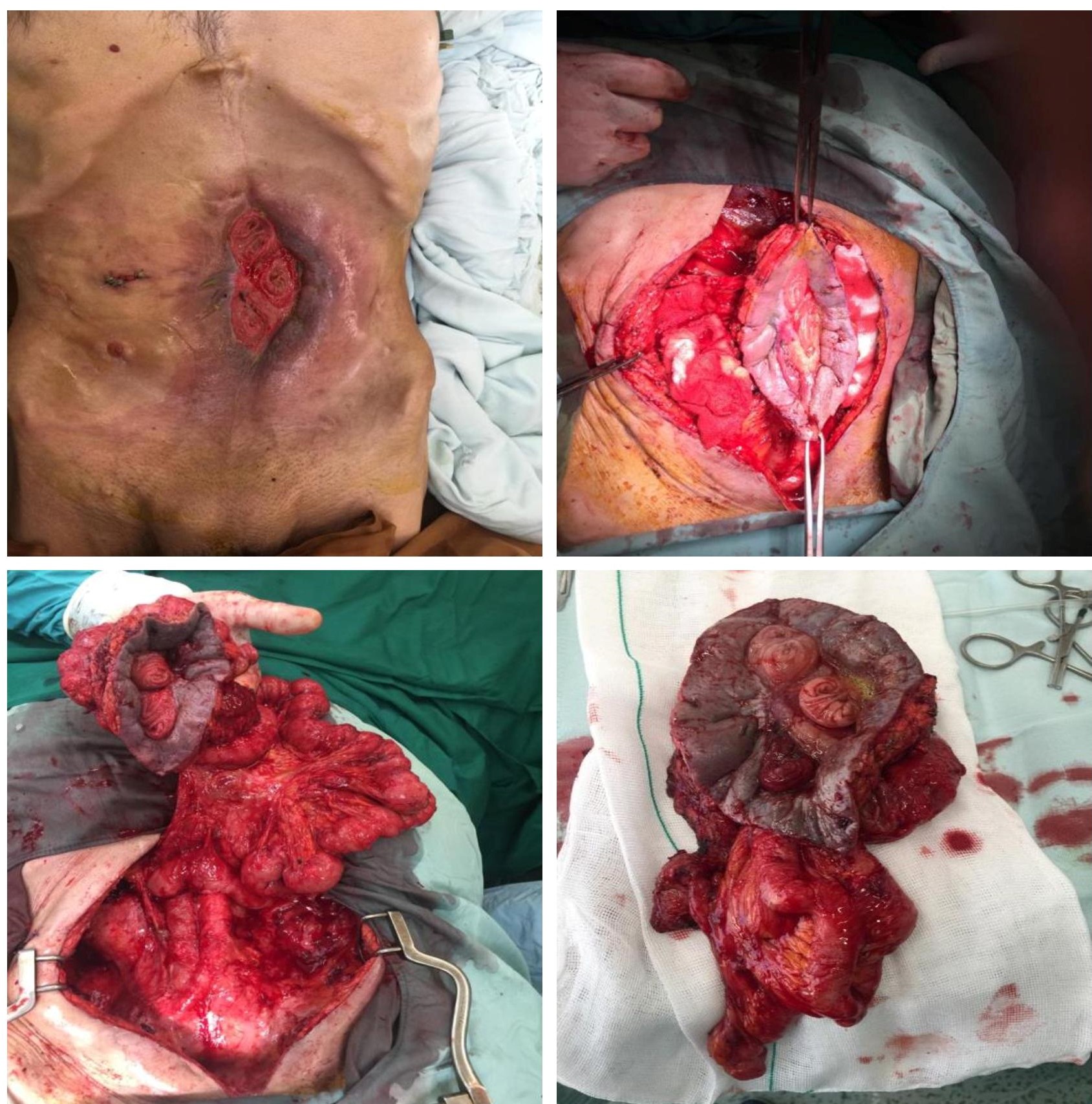
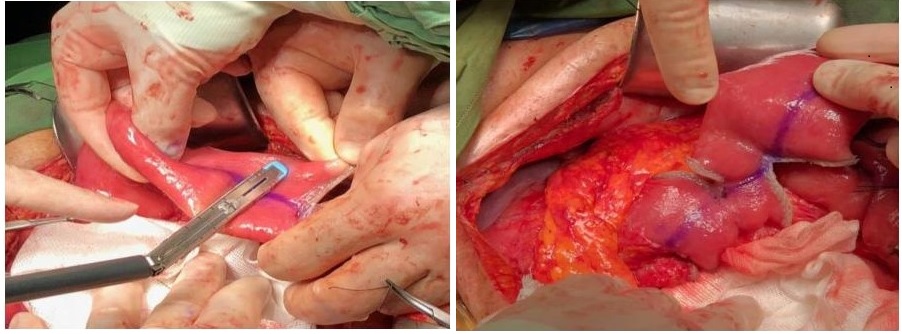
Discussion: By establishing the first IRU in our center and practicing AGIR we have been able to achieve intestinal autonomy in patients suffering from IF, reduce the number of the candidates for intestinal transplantation, and reduce mortality rates.
Conclusion: This series introduced the results of a multidisciplinary program for the treatment of IF in a middle-income country that lacks facilities for HPN. Our report shows a successful experience with the management of patients with IF by establishing an intestinal failure, rehabilitation and transplant unit in a country that lacks facilities for HPN.
There are no comments yet...