Humanized von Willebrand factor reduces platelet sequestration in pig xenogeneic lung perfusion and pig-to-primate lung transplantation
Margaret Connolly1, Lars Burdorf1, Zahra Abady1, Kaitlyn Petitpas1, Selin Sendil3, Carol Phelps2, Kasinath Kuravi2, David Ayares2, Agnes Azimzadeh1, Richard N. Pierson III1.
1Center for Transplantation Sciences, Massachusetts General Hospital, Boston, MA, United States; 2Revivicor, Inc, Revivicor, Blacksburg, VA, United States; 3Department of Surgery, University of Maryland, Baltimore, MD, United States
Introduction: Von Willebrand factor (vWF) is an important element of hemostasis and when activated, mediates hemostasis via platelet adhesion and aggregation under shear stress conditions. Porcine vWF (pvWF) behaves as if “always active” when exposed to human blood, leading to non-physiologic platelet adhesion and activation. We hypothesized that pig lungs expressing humanized vWF (hvWF) would exhibit attenuated platelet sequestration and activation.
Materials and Methods: GalTKO.hCD46.hvWF transgenic lungs, in which a region containing the GP1b-binding domain of the porcine vWF gene was replaced with the cDNA of several human ortholog sequences, were perfused in an ex vivo model with freshly collected human blood and compared to reference GalTKO.hCD46 lungs, lacking the vWF modification; 1-BIA (thromboxane synthase inhibitor), anti-GPIb Fab, and histamine receptor blockade were used in all experiments. Blood perfusing one lung from each pair of lungs (n=5 hvWF, n=5 reference) was ‘treated’ with an integrin (H52/IB4) and selectin (GMI-1271, PSGL-1) blocking cocktail. Experiments were terminated electively after 8 hours of perfusion if lungs had not failed earlier. Platelet counts were measured by flow cytometry. GalTKO.hCD46.hvWF transgenic lungs were also used for transplantation into baboon recipients (n=4 hvWF, n=10 reference), with platelet counts measured by CBC.
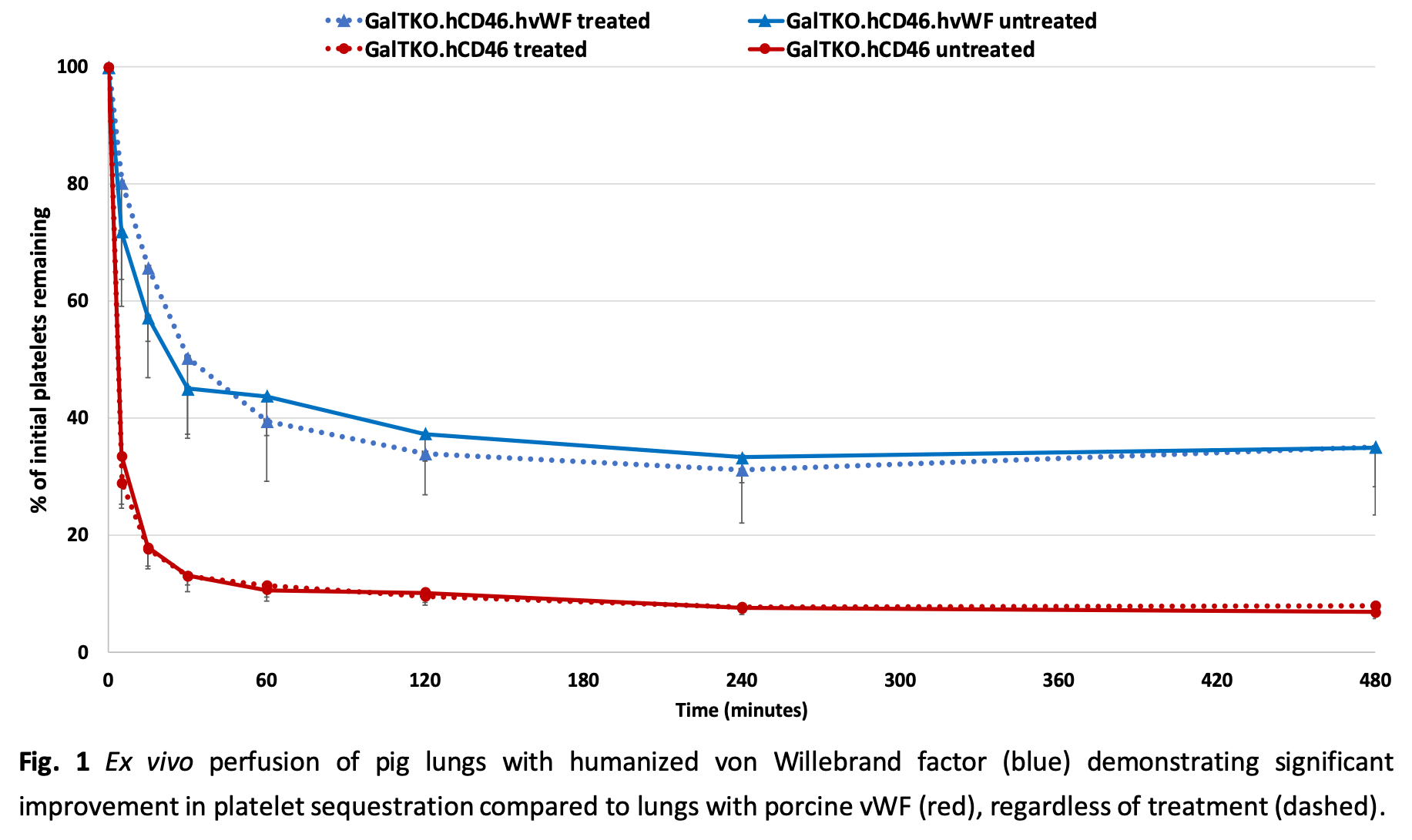
Results: All ex vivo groups showed similar survival time, with most experiments electively terminated at 8 hrs. Pulmonary vascular resistance remained very low and constant in both cohorts. Platelet sequestration was significantly reduced and delayed in lungs with hvWF compared to those with pvWF, and was not further modulated by selectin and integrin blockade (p<0.01) (Fig.1).
No significant differences were observed in BTG (platelet activation marker) levels, F1+2 (thrombosis marker) levels, and neutrophil counts. Baboons that received hvWF lungs survived longer with attenuated thrombocytopenia compared to those receiving the reference lungs (p<0.01) (Fig. 2).
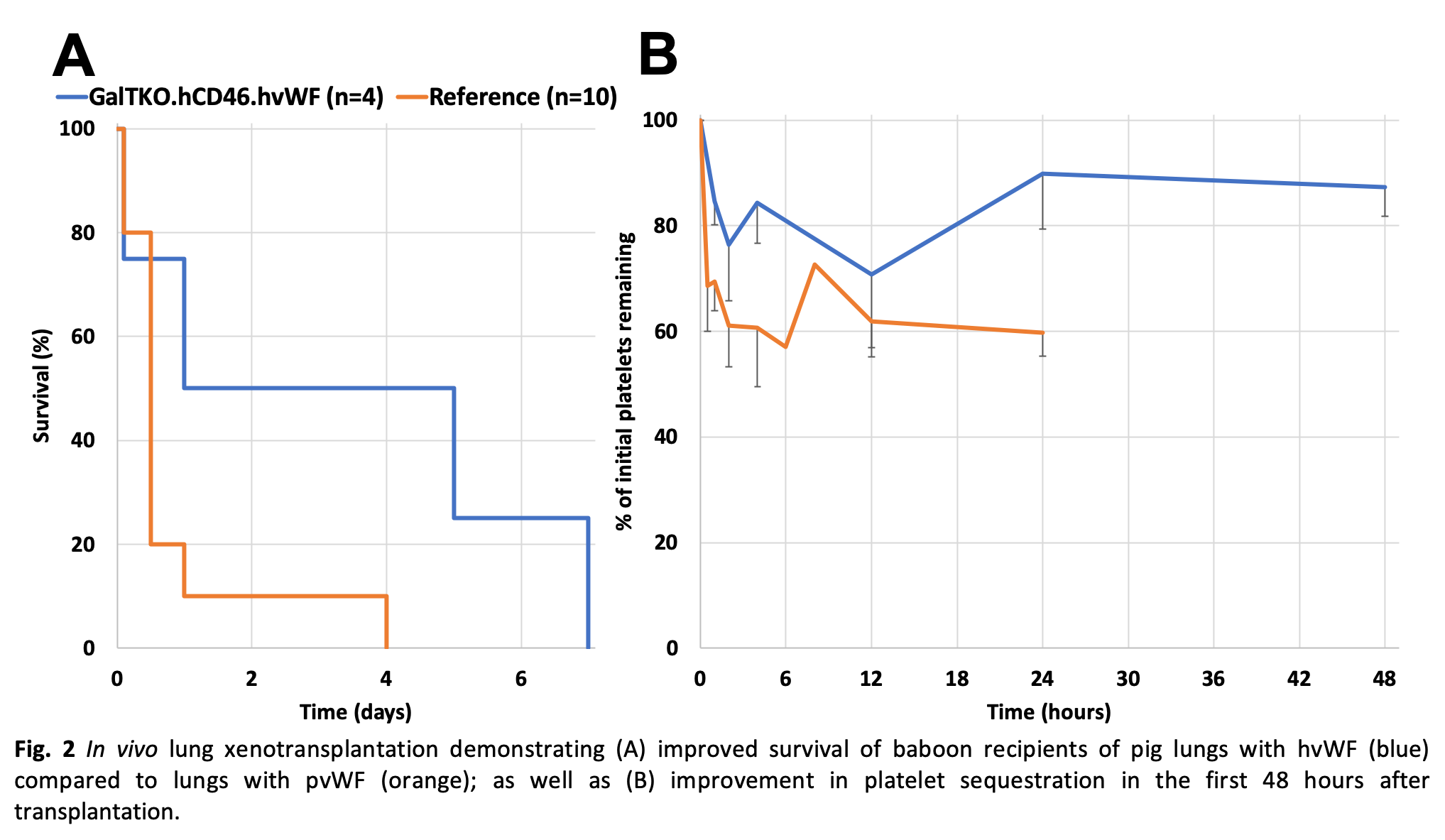
Discussion: When perfused with human blood, pig lungs with humanized vWF had reduced sequestration of platelets compared to lungs with porcine vWF under identical ex vivo perfusion conditions. Similar reductions were seen when the hvWF pig lungs were transplanted into baboon recipients.
Conclusion: “Humanization” of porcine vWF attenuates the non-physiologic platelet adhesion and aggregation associated with xenograft rejection in both ex vivo and in vivo models. Current work to identify selectin- and integrin-independent platelet adhesion mechanisms will focus on Fc-receptors, adenosine pathway dysregulation, activated neutrophils, and coagulation pathway dysregulation, through additional drug treatments and genetic modifications.
Supported by NIH U19 AI090959. Supported by unrestricted educational gifts from United Therapeutics/ Lung Biotechnology LLC.
